Mullerian Anomalies Showing Variety of Clinical Scenarios: Case Series
* Megha Kansara;
Meenakshi Gothwal;
Garima Yadav;
Pratibha Singh;
Priyanka Kathuriy;
-
* Megha Kansara: Department of Obstetrics and Gynecology, AIIMS, Jodhpur, Rajasthan 342005, India.
-
Meenakshi Gothwal: Department of Obstetrics and Gynecology, AIIMS, Jodhpur, Rajasthan 342005, India.
-
Garima Yadav: Department of Obstetrics and Gynecology, AIIMS, Jodhpur, Rajasthan 342005, India.
-
Pratibha Singh: Department of Obstetrics and Gynecology, AIIMS, Jodhpur, Rajasthan 342005, India.
-
Priyanka Kathuriy: Department of Obstetrics and Gynecology, AIIMS, Jodhpur, Rajasthan 342005, India.
-
Feb 07, 2022 |
-
Volume: 1 |
-
Issue: 1 |
-
Views: 2302 |
-
Downloads: 1659 |
Abstract
Mullerian anomalies of the female genital tract cause a variety of pathologies, adversely affecting a woman’s health. Here, we, showing five cases, highlighting different clinical scenarios, diagnosis, and management.
- A 16-year-old girl with the uni-cornuate uterus and atretic non-communicating one cervix and associated renal anomaly.
- A 27-year-old woman with OHVIRA (Obstructed Hemi-Vagina with Ipsilateral Renal Anomaly) syndrome.
- A 25-year-old woman with a uterine malformation on HSG as an incidental finding.
- A 16-year-old girl with a bicornuate uterus with a rudimentary non-communicating left horn.
- A 19-year-old girl with MRKH (Mayer Rokitansky Kuster Hauser Syndrome) syndrome. Mullerian anomalies may show various symptoms/signs, and clinicians should be aware of this condition.
Correct diagnosis and appropriate management are necessary. Congenital anomalies of the female reproductive tract may involve the uterus, cervix, fallopian tubes, or vagina. A woman’s obstetric and gynecologic health may be adversely affected depending on the specific defect. In this manuscript, we will present a series of five cases with different clinical scenarios, their diagnosis, and management - The first patient is a 16-year-old adolescent girl with normal menstruation with the unicornuate uterus and atretic non-communicating one cervix and associated renal anomaly. The second patient is a 27 year P1001 fertile older woman with a rare case of OHVIRA syndrome. The third case is a 25-year woman who presented with secondary infertility with a uterine malformation on HSG (Hysterosalpingography) as an incidental finding. The fourth case is an about 16-year-old girl who presented to our gynecological OPD with complaints of severe dysmenorrhoea since menarche and Magnetic Resonance Imaging (MRI) report of bicornuate uterus with rudimentary non- communicating left horn. The fifth case is about a 19-year-old girl who came with primary amenorrhea and an MRI report of MRKH syndrome for which vaginoplasty was done. Our study aims to elaborate on Mullerian anomalies’ different clinical manifestations, making their correct diagnosis and appropriate management to improve the obstetric and gynecological outcome.
Introduction
Congenital uterine malformations result from abnormal formation, fusion, or reabsorption of the Mullerian ducts during fetal life. Fusion defects result from the incomplete merging of the caudal portion with the Mullerian ducts (lateral fusion) or incomplete merging of the structures of the urogenital sinus with the Mullerian tubercle (vertical fusion). Failures in lateral fusion may result in uterus didelphys, bicornuate uterus, or arcuate uterus. When the defect occurs in vertical fusion, anomalies such as imperforate hymen, transverse vaginal septum, oblique vaginal septum, or absence of the cervix may result. Following caudal fusion of the ducts, the remaining portion of the central septum is reabsorbed. Reabsorption failure results in a uterus with a partial or complete septum. Certain malformations of the uterine cavity also lead to the formation of the hypo-plastic uterus, infantile uterus, agenesis of the cervix, and T-shaped uterus [1]. Their cause has yet to be fully clarified, and it is currently believed to be multifactorial. Mullerian malformations have an estimated incidence of 1.1%–3.5% [2]. Septate uterus is the commonest uterine anomaly with a mean incidence of ~35%, followed by bicornuate uterus (~25%) and arcuate uterus (~20%) [3]. Unicornate and didelphys uterus have term delivery rates of ~45%, and the pregnancy outcome of patients with an untreated bicornuate and septate uterus is also poor, with term delivery rates of only ~40% [3]. The arcuate uterus is associated with a slightly better but still impaired pregnancy outcome with term delivery rates of ~65% [3]. ESHRE classification is the latest classification system used as it also classifies vaginal anomalies apart from the uterus and cervix [4].
Mullerian anomalies may lead to age-related symptoms such as cyclical pelvic pain, primary amenorrhoea, prolonged or otherwise abnormal bleeding at the time of menarche and infertility, recurrent pregnancy loss, abnormal presentation, premature delivery in the reproductive age group and thus may be identified in girls and women who present with these disorders. Some may be suspected because of associated findings on physical examination, such as a longitudinal vaginal septum. Others may be detected when imaging studies are performed to evaluate patients with infertility, symptoms related to non-reproductive organ systems, or trauma. A unicorn ate uterus is seldom symptomatic unless associated with other malformations. If a rudimentary, non-communicating uterine horn is present together with a functional endometrium, hematometra and sometimes hematosalpinges may be found [5]. Anomalies resulting from failure in vertical fusion, such as cervical agenesis, transverse vaginal septum, and imperforate hymen, are associated with primary amenorrhea, hematocolpos, and hematometra [6]. Renal tract anomalies have been detected in 30%–41% of women with specific uterine anomalies such as uterine agenesis and unicornuate uterus [7,8]. There are several techniques available to evaluate uterine malformations. When the cavity only is to be assessed, Hysterosalpingography (HSG) and hysteroscopy are especially useful. Laparoscopy is best for examination of the uterine fundus. Nowadays, 3D ultrasound and MRI can make the correct diagnosis and are more specific. Ultrasound is quick, readily available, and cheap, and lacks radiation. However, image degradation can occur with large patients, overlying bowel gas, and the external contour may be difficult to visualize. Three-dimensional (3D) ultrasound is a new technique that has shown inexperienced hands to be more accurate than two-dimensional ultrasound and equal or better than MRI at assessing Mullerian development anomalies [9]. MRI is the modality of choice because of its high accuracy in detecting and accurately characterizing Mullerian duct anomalies. It lacks radiation and provides a clear delineation of both the internal and the external uterine anatomy.
The following five clinical cases we encountered at our institution.
Case Presentation 1
The 16-year-old unmarried girl presented to our OPD with complaints of pain right lower abdomen for one year. She had her menarche at 14 years, her last menstrual period was February 26, 2019, cycles were regular, and there were no other menstrual complaints. On examination, her vitals were stable. Per abdominal examination, the abdomen was soft, and there was no organomegaly. Her secondary sexual characteristics were well developed. She had her ultrasound finding suggestive of an absent right-sided kidney with right sided ovarian cyst of 6 cm × 5 cm. She was subjected to MRI pelvis (Figure 1) in which there was absent right kidney, bicornuate uterus with a single upper vagina, left-sided cervix, uterine body, fallopian tube, and left ovary were normal, atretic hypoplastic right cervix (non-communicating with a vagina) with right hematometra of 3.4 cm × 2.6 cm × 2.7 cm, right hematosalpinx is of size 5.8 cm × 5.7 cm × 5.6 cm and normal right ovary. Since the patient was symptomatic for one year, we planned her for diagnostic laparoscopy after consent and pre-operative workup.

On laparoscopy, the findings were:
- Left hemi-uterus with left tube, ovary & round ligament visualized in the pelvis (Left side).
- On the right side, the accessory non-communicating horn of the uterus with tubes dilated (8 cm × 8 cm) and normal ovary seen attached to the lateral pelvic wall. Omentum has adhered to the uterus’ accessory horn–adhesiolysis done by sharp & blunt dissection.
- Right salpingectomy done and right horn excised.
Her post-operative period was uneventful, and she was discharged on day 2. In this case, the cause of the pain was functioning non-communicating right uterine horn, leading to the collection in tubes. The patient was relieved of pain and is under follow-up to date.
Case Presentation 2
A 27-year-old woman presented to our OPD with complaints of spasmodic dysmenorrhoea since menarche. She had her menarche at 13 years of age, and her cycles were regular, and there were no menstrual complaints. She had one child one year back by cesarean section, indicating didelphys uterus. She also had a history of left-sided open nephrectomy with left ovariotomy two years back, indicating left kidney failure with associated ovarian cyst. On examination, her vitals were stable, chest and cardiovascular examination were normal, on per abdominal examination, her abdomen was soft and no organomegaly. The bulge was present on the left anterolateral wall, a single cervical opening seen posteriorly on per speculum examination. Per vaginal examination, cervix felt posterior to bulge, and uterine size could not be well assessed. Findings of her ultrasound report were absent left kidney, right kidney compensatory enlarged, right ovary normal, left ovary was absent, uterine didelphys, right horn draining into patent right hemivagina. In contrast, the left horn is draining into the left obstructed hemivagina with a blood clot of 50 cc–60 cc collection. These findings suggest OHVIRA with uterine didelphys.
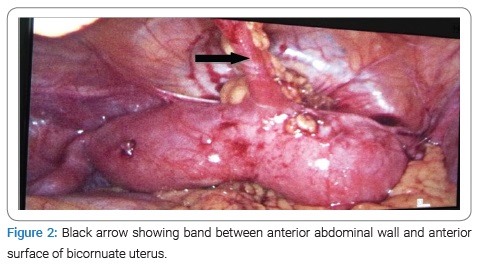
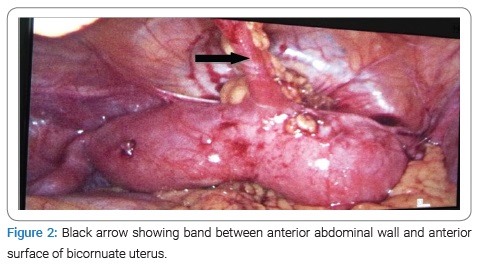
On laparoscopy, the findings (Figure 2) were:
- Bicornuate uterus with right horn larger than left.
- Flimsy adhesions were present between the anterior abdominal wall and omentum.
- Right ovary and fallopian tube were normal.
- Left ovary not seen.
- 1 cm broadband attaching anterior wall of the uterus with anterior abdominal wall with the anterior surface wall.
Vaginaly gave Stab incision on most bulging part 20 cc–40 cc blood drained and the second cervical opening was seen separately (Figure 3).

Longitudinal septum in between two vaginae excised .and postoperatively both cervical openings seen. On hysteroscopy done through left cervix-left uterine cavity and cervix were normal-looking Foleys catheter was placed inside the vagina. The postoperative period was uneventful, and foleys were removed on day 4. The patient improved symptomatically, and she was discharged on day 5. In this case, the diagnosis of obstructed hemivagina, uterine didelphys, and the ipsilateral renal anomaly was confirmed postoperatively.
Case Presentation 3
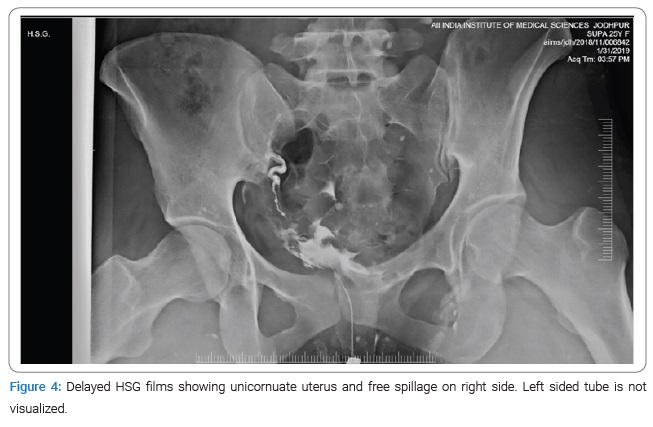
A 25-year-old woman presented to our OPD with secondary infertility, anxious to conceive. She was married for eight years and had one term vaginal delivery five years back, but the baby expired due to some congenital anomaly in the brain. She has been trying to conceive since then. She did not have any menstrual complaints; her cycles were regular. She did not have a history of tuberculosis, diabetes, hypothyroidism. On examination, her vitals were stable, and general physical and systemic examination was normal. She was subjected to routine workup for infertility. Her blood investigations and hormonal profile were normal. Menstrual blood TB PCR was negative, and husband semen analysis was also normal. Her hysterosalpingography (Figure 4) showed a unicornuate uterus with right-sided fimbrial and left corneal blocks. We planned this patient for diagnostic laparo-hysteroscopy and chromopertubation.
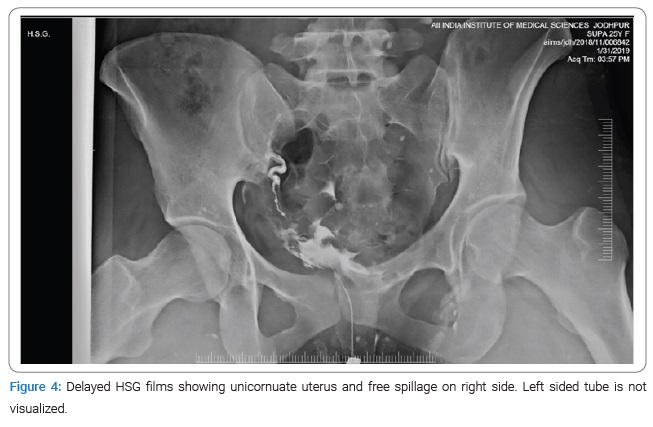
On laparoscopy, the findings were:
- Upper abdomen was normal
- Unicornuate uterus with right-sided tube and ovary normal.
- Left-sided non -communicating rudimentary horn, which was non-functioning with left-sided tube and ovary normal looking.
- On the chromopertubation test, right-sided spill was present, and left-sided spillage was absent.
After the above findings on laparoscopy, we counseled the patient regarding the cause of decreased fertility of one tube and chances of conception through another tube. As a result, we discharged her on postoperative day two and planned her for ovulation-induction in the next cycle.
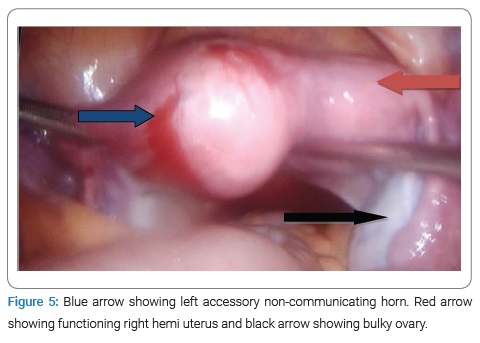
Case Presentation 4
A 16-year-old girl presented to our gynecological OPD with complaints of severe dysmenorrhoea since menarche. She had her menarche at 14 years of age; her cycles were infrequent, coming at the duration of 2 months lasting for four days, average flow, associated with severe dysmenorrhoea. On examination, her vitals were stable, and secondary sexual characters were well developed. Her BMI was 26 kg/m2 breast, pubic hair, and axillary hairs were well developed. There was no clinical hirsutism and galactorrhea. On local examination, external genital organs were well developed. Blood investigations and hormonal profiles were normal. There was a unicornuate uterus on ultrasound with a functioning left rudimentary horn and echogenic fluid collection in the endometrial cavity, the possibility of ACUM (Accessory and Cavitated Uterine Mass). On MRI, the findings were bicornuate uterus with rudimentary left horn with blood clots in it, apparently stenosed Ostia communicating rudimentary horn with right horn-single cervix and bilateral polycystic ovaries.
To confirm the diagnosis, we did diagnostic laparoscopy, and the findings (Figure 5) were as follows:
- Right functioning Hemi uterus.
- Left accessory functioning uterine mass (non-communicating with right horn).
- Bilateral polycystic ovaries.
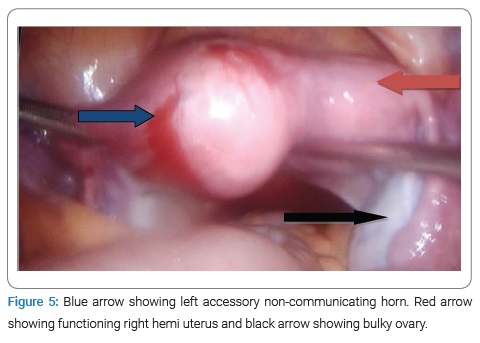
Since the left accessory uterine mass was non-communicating and there was a collection, the patient was symptomatic; the left horn was removed.
In the postoperative period, her vitals were stable, and she was discharged on post-op day 2 in satisfactory condition, and she was symptomatically improved and followed up to date.
Case Presentation 5
The 19-year-old married nulliparous woman came with primary amenorrhoea. She has been married for three months, and she has complained of difficulty in sexual intercourse since then. There was no history of cyclical pain abdomen or abdominal lump.
There was no history of similar complaints in mother and sister. On examination, her secondary sexual characteristics were well developed, there was no abdominal or inguinal swelling, and external genital organs were well developed. Per vaginal examination, there is a blind vaginal pouch of one centimeter, and the cervix is not felt. On MRI, uterus, cervix, and upper vagina were absent, bilateral ovaries were normal and bilateral kidneys were normal. Since the woman is diagnosed to have MRKH, we counseled her regarding her fertility options and sexual function.
She was planned for vaginoplasty with skin grafting after routine preoperative investigation and work up. She was discharged on postoperative day eight and followed up to date.
Discussion
Most Mullerian Duct Anomalies (MDAs) are associated with functioning ovaries and age-appropriate external genitalia. These abnormalities are often recognized after the onset of puberty. In the prepubertal period, normal external genitalia and age-appropriate developmental milestones often mask abnormalities of the internal reproductive organs. After puberty, young women often present to the gynecologist with menstrual disorders. Late presentations include infertility and obstetric complications. The actual incidence of Mullerian anomalies in the general population is unknown. Most authors report incidences of 0.1%–3.5% [1–3]. In 2001, Grimbizis and colleagues reported that the mean incidence of uterine malformations was 4.3% for the general population and fertile women [3]. When these data are obtained in women with recurrent pregnancy loss who are undergoing hysterosalpingography (HSG), the prevalence of Mullerian anomalies is 8%–10% [10]. Many patients with uterine anomalies are asymptomatic and found accidentally during a routine pelvic examination or during pregnancy using 2D ultrasound [11]. Women with uterine anomalies have high cesarean section rates, mainly caused by fetal malpresentation [11]. Hysterosalpingography, 2D ultrasound, and endoscopies were mostly used to diagnose female genital tract anomalies. Nowadays, non-invasive imaging techniques such as 3D ultrasound and MRI are the recommended procedures for diagnosing Mullerian duct anomalies [12].
The Triad of uterine didelphys obstructed hemivagina and unilateral renal agenesis is called OHVIRA syndrome or Herlyn-Werner-Wunderlich syndrome. OHVIRA syndrome has an incidence of 0.16%–3.8% of these Mullerian anomalies [13]. The most common clinical presentation is pelvic pain initiated shortly after the menarche associated with a vaginal or pelvic mass and normal menstrual periods. The didelphys uterus, in these cases, is associated with obstetric complications such as miscarriages, preterm labor, and placental dysfunction. Rare presentations may include intermenstrual bleeding, acute urine retention, fever, vomiting, and abdominal swelling. The menstrual flow that comes from the unobstructed patent hemivagina gives the impression of normal menses. Consequently, accurate diagnosis and surgical treatment may be delayed for several months or even years. Imaging modalities used to diagnose this condition include ultrasonography and MRI. Computed Tomography (CT) has a limited role in evaluating the female pelvis. The obstructing vaginal septum seen in this condition is usually oblique and varies in thickness from very thin to quite thick. Resection of the vaginal septum is the treatment of choice to relieve obstructing symptoms.
Mullerian anomalies consist of many defects that may vary from patient to patient. Therefore, their management must also be individual, considering anatomical and clinical characteristics and the patient’s wishes.
Acknowledgment
I would like to acknowledge my co-authors for constantly inspiring me, my teachers, parents and friends.
Conflict of Interest
There is no conflict of interest between authors and the article is only sent in this journal.
References
- Golan A, Langer R, Bukovsky I, Caspi E. Congenital anomalies of the müllerian system. Fertil Steril. 1989;51(5):747–755.
- Strassmann EO. Fertility and unification of double uterus. Fertil Steril. 1966;17(2):165–176.
- Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update. 2001;7(2):161–174.
- Grimbizis GF, Gordts S, Di Spiezio Sardo A, Brucker S, De Angelis C, Gergolet M, et al. The ESHRE/ESGE consensus on the classification of female genital tract congenital anomalies. Hum Reprod. 2013;28(8):2032–2044.
- Johansen K. Pregnancy in a rudimentary horn. Two case reports. Obstet Gynecol. 1969;34(6):805–808.
- Nawroth F, Schmidt T, Freise C, Foth D, Römer T. Is it possible to recommend an “optimal” postoperative management after hysteroscopic metroplasty? A retrospective study with 52 infertile patients showing a septate uterus. Acta Obstet Gynecol Scand. 2002;81(1):55–57.
- Fedele L, Bianchi S, Agnoli B, Tozzi L, Vignali M. Urinary tract anomalies associated with unicornuate uterus. Urology. 1996;155(3):847–848.
- Oppelt PG, Lermann J, Strick R, Dittrich R, Strissel P, Rettig I, et al. Malformations in a cohort of 284 women with Mayer-Rokitansky-Küster-Hauser syndrome (MRKH). Reprod Biol Endocrinol. 2012;10:57.
- Deutch TD, Abuhamad AZ. The role of 3-dimensional ultrasonography and magnetic resonance imaging in the diagnosis of müllerian duct anomalies: a review of the literature. J Ultrasound Med. 2008;27(3):413–423.
- Youssef MA. Obstructed hemivagina and ipsilateral renal anomaly syndrome with uterus didelphys (OHVIRA). Middle East Fertil Soc J. 2013;2012(12):004.
- Chan YY, Jayaprakasan K, Tan A, Thornton JG, Coomarasamy A, Raine-Fenning NJ. Reproductive outcomes in women with congenital uterine anomalies: a systematic review. Ultrasound Obstet Gynecol. 2011;38(4):371–382.
- Grimbizis GF, Di Spiezio Sardo A, Saravelos SH, Gordts S, Exacoustos C, Van Schoubroeck D, et al. The Thessaloniki ESHRE/ ESGE consensus on diagnosis of female genital anomalies. Gynecol Surg. 2016;13:1–16.
- Smith NA, Laufer MR. Obstructed hemivagina and ipsilateral renal anomaly (OHVIRA) syndrome: Management and follow-up. Fertil Steril. 2007;87(4):918–922.
Keywords
Mullerian anomalies; MRKH syndrome; OHVIRA; Vaginoplasty
Cite this article
Kansara M, Gothwal M, Yadav G, Singh P, Kathuriya P. Mullerian anomalies showing variety of clinical scenarios: case series. Glob J Gynecol Obstet Res. 2022;1(1):1–6.
Copyright
© 2022 Megha Kansara. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).