Abstract
The Pleomorphic Adenoma (PA) is the commonest neoplasm of the major salivary glands. Palate is commonest site amongst the pleomorphic adenoma of minor salivary glands. However, they can also occur in the larynx, trachea, and floor of mouth, upper lip and cheek. In this report, we are presenting a relatively rare case of pleomorphic adenoma of the minor salivary glands of tonsil which was treated surgically with no recurrence till fourteen months of follow-up.
Introduction
PA is the commonest neoplasm of the major salivary glands. The name pleomorphic adenoma is based on the architectural pleomorphism seen on light microscopy [1]. Minor salivary gland tumors are relatively uncommon, accounting for only 10% to 25% of all salivary glands tumors. Also, most of the minor salivary gland tumors are malignant unlike those in the major salivary glands [2]. Palate is commonest site amongst the PA of minor salivary glands. However, they can also occur in the larynx, trachea, and floor of mouth, upper lip and cheek [3]. The aim of this paper is to describe a case of PA of minor salivary gland of the tonsil which is a rare entity with very few reported cases [4,5].
Case Report
A 50-year-old lady came to the ENT outpatient department of Gandaki Medical College with complaint of foreign body sensation in throat for the last 3 months. She also had difficulty in swallowing and speaking. There was no history of fever, pain in throat, loss of appetite, weight loss, chronic cough, hemoptysis, change in voice, hematemesis or any history of surgical procedure in the throat or neck in the past. She had no known co-morbidity. She was a non-smoker and she was not under any medication.
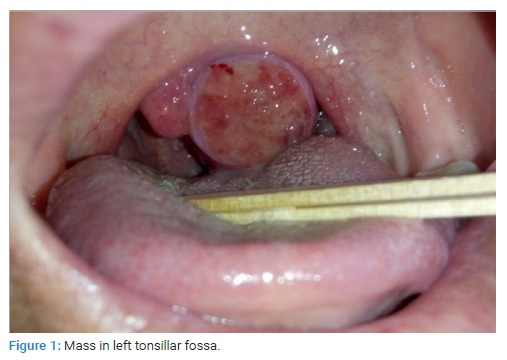
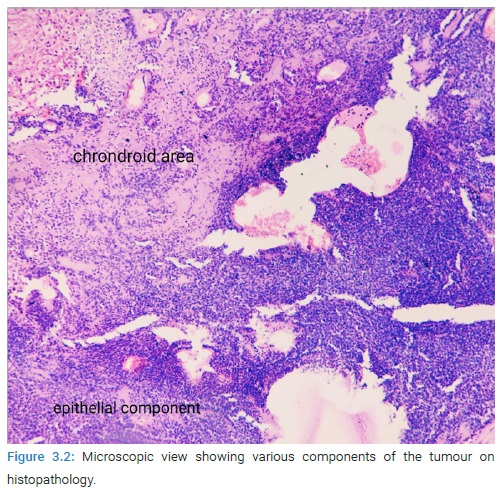
On examination, her general condition was fair. There was a single, red, fleshy, non-pulsatile, sessile, lobulated mass with ulcerated mucosa on the left tonsillar fossa crossing the midline and pushing the uvula to the contralateral side (Figure 1). On palpation, it was non tender, firm, well-defined and bled on touch. Left tonsil couldn’t be identified separately. The right tonsil appeared normal. There were no palpable neck nodes.
Keeping in view the history and clinical findings, we made a list of differential diagnosis including left tonsillar malignancy (squamous cell carcinoma/lymphoma), left tonsillar papilloma, left tonsillar cyst, tumor from deep lobe of left parotid gland extending into the tonsillar fossa, left parapharyngeal space tumor.
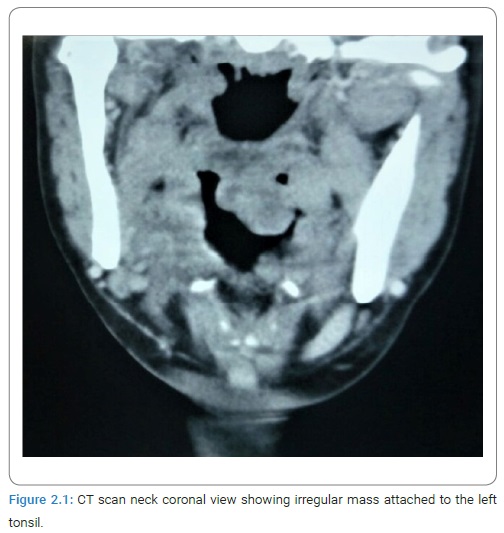
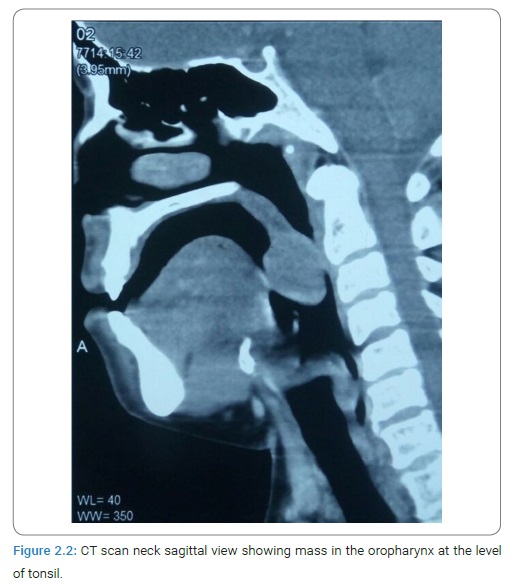
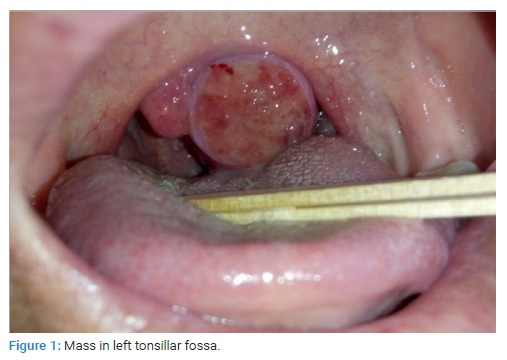
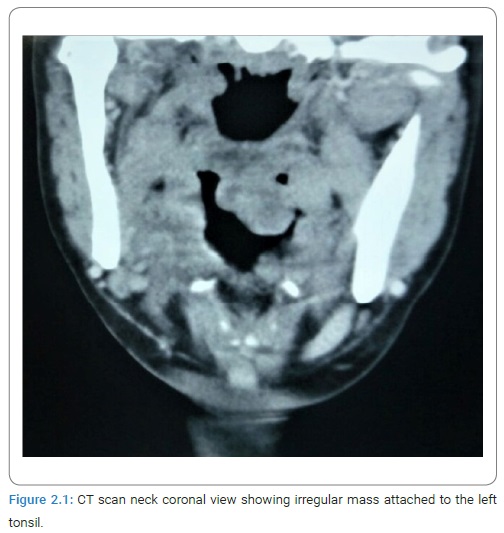
Contrast enhanced CT scan of her neck showed a heterogeneously enhancing soft tissue lesion of approximately 2.2 cm × 2.5 cm × 2.1 cm size over the left tonsillar fossa with normal appearing cervical lymph nodes (Figure 2.1 and Figure 2.2).
She underwent left tonsillectomy under general anesthesia for biopsy purpose. Peroperatively, the mass was attached to the medial tonsillar surface and was removed in-toto along with the left tonsil. There was no unusual bleeding during the procedure.
After an uneventful postoperative period of 3 days, she was discharged and asked to follow-up with histopathology report.
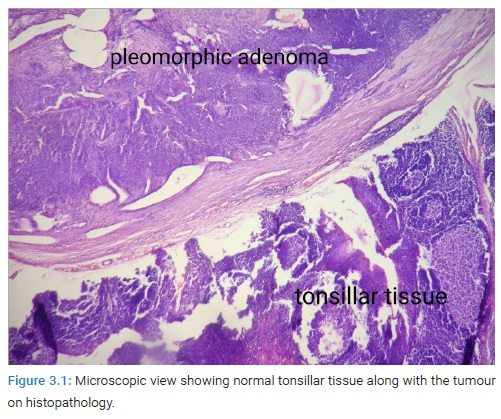
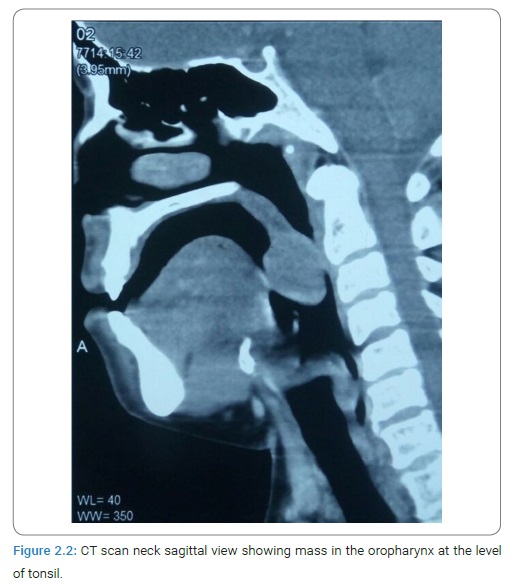
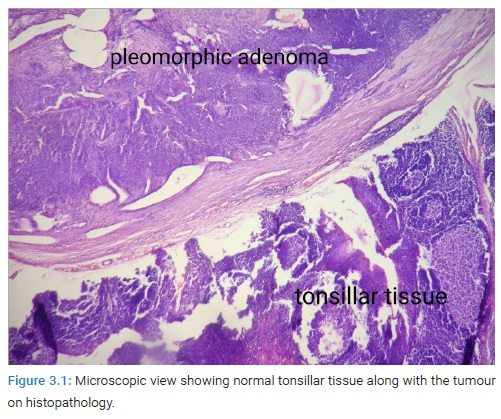
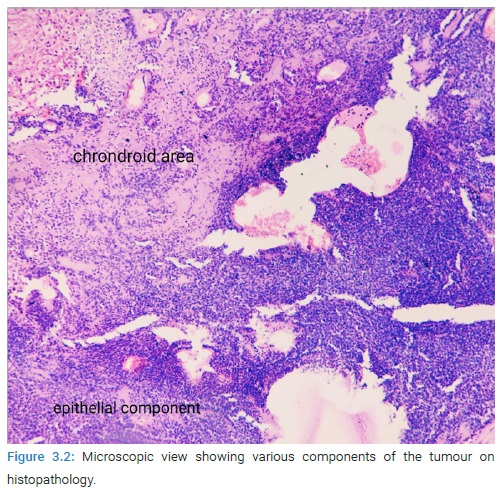
Histopathology report came out to be pleomorphic adenoma of minor salivary gland of tonsil (Figure 3.1 and Figure 3.2).
She is on regular follow-up for the last 14 months with no signs of recurrence.
Discussion
PA as the name suggests, shows architectural pleomorphism on light microscopy. PA accounts for 73% of all salivary gland tumors [6].
In a study by Spiro et al. [7] on 2078 patients with salivary gland neoplasia, most of the patients with PA were in their 4th to 6th decade of life, women being the more commonly affected [7].
Of the very few reported cases of PA of minor salivary glands of tonsil, one was by Pothula et al. [4] in a 54-year-old patient and another by Mahore et al [5]. in a 45-year-old patient, both being females. The duration of symptoms ranged from few months to few years. The symptoms spectrum included choking sensation, dysphagia, neck pain, ear block, nose block, recurrent sore throat [4,5]. Our patient had foreign body sensation in throat and dysphagia.
Palate is the commonest site affected amongst the minor salivary glands. However, they can also occur in the larynx, trachea, and floor of mouth, retromolar trigone, upper lip and cheek [7–9].
PA is a well circumscribed, benign neoplasm which is oval or round. Cystic degeneration or the presence of chondroid/osteoid tissues makes the consistency either soft and fluctuant or firm and rubbery [10]. The tumor comprises of mesenchymal, epithelial and myoepithelial components complexly arranged. The epithelial cells produce glandular and ductal components containing eosinophilic content. Keratin pearls and squamous metaplasia are also present. Distinct features of PA are myoepithelial cells, with clear cells, spindle cells and oxyphilic cells also found frequently. Chondroid, myxoid and osseous areas are made by the mesenchymal element of the tissue. A false capsule is generally present as a result of fibrosis of the salivary gland parenchyma [11].
Surgical excision is the treatment of choice [12–13]. Sometimes the capsule is breached by microscopic pseudopod-like extensions. As a result, rupture of the capsule, inadequate resection or tumor spillage during excision can lead to local recurrence [14]. Up to 6% of patients have been reported to have recurrence [5]. Late recurrence and malignant transformation has been reported, hence long-term follow-up is mandatory [15].
Conclusion
Pleomorphic adenoma (PA) is the commonest neoplasm of salivary glands, major salivary glands being mostly involved. PA of minor salivary glands of tonsil is among the rarest and least reported cases. The symptomatology varies from dysphagia, foreign body sensation in throat to pain in neck, ear block and recurrent sore throat. The goal of treatment is complete surgical excision and regular long term follow-up as this tumor is notorious for late recurrence.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Pleomorphic adenoma; Minor salivary glands; Tonsil
Cite this article
Neeraj KC, Rajendra N, Sunita R. Pleomorphic adenoma of the palatine tonsil: a rare entity. World J Public Health Epidemiol. 2022;1(1):1–3.
Copyright
© 2022 Neeraj KC. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).