Abstract
A Carotid Body Tumor (CBT) is a rare tumor of neural crest cell origin that is mostly located at the carotid bifurcation. We present a case of asymptomatic bilateral sporadic CBT with a 2 cm X 2 cm pulsatile, firm, non-tender swelling was found in the right side of the neck at the level II region. Imaging confirmed the diagnosis and then removed it surgically. Biopsy of mass is nonmalignant and the patient is under follow-up. So, we report clinical suspicion, imaging findings, and histological findings in the case.
Introduction
A CBT is a rare tumor originating from neural crest cells. The majority of paragangliomas are discovered between the third and fifth decades of life. It is very uncommon in children. It can present as familial;10% with bilateral tumors seen in 32% of cases, or sporadic; mostly unilateral and in only 5% of the patients [1]. The vast majority of these tumors are benign, with about 2%–13% developing into malignant tumors that can spread to regional lymph nodes, lungs, and bones. Clinical assessment is important to identify CBT. Since the tumor is vascular in origin, imaging (USG, CT/MRI, or angiography) is mostly used for the diagnosis. A CBT is separated from other neck masses based on vascularity and location. A biopsy is not suitable for diagnosis unless malignancy is suspected due to its vascular origin [1].
Case Presentation
A 33-year female presented with a right-sided neck mass for 5 months. The patient was asymptomatic and there was no associated pain, dysphagia or features of lower cranial nerve paralysis ruling out compression of the adjoining structures. Symptoms suggestive of hypercatecholenemia like palpitation, hypertension or perspiration were not present. On examination, a 2 cm X 2 cm pulsatile, firm, non-tender swelling was found in the right side of the neck at the level II region (Figure 1).

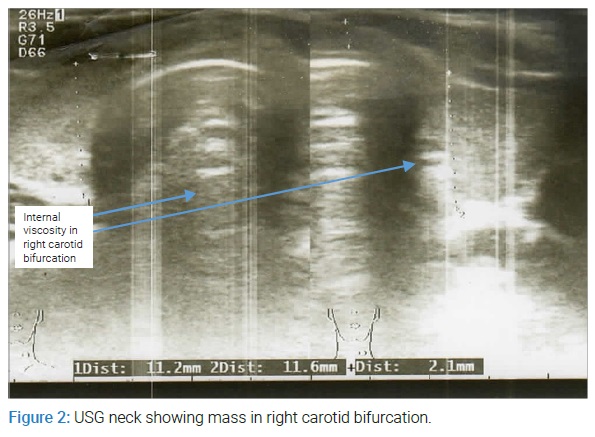
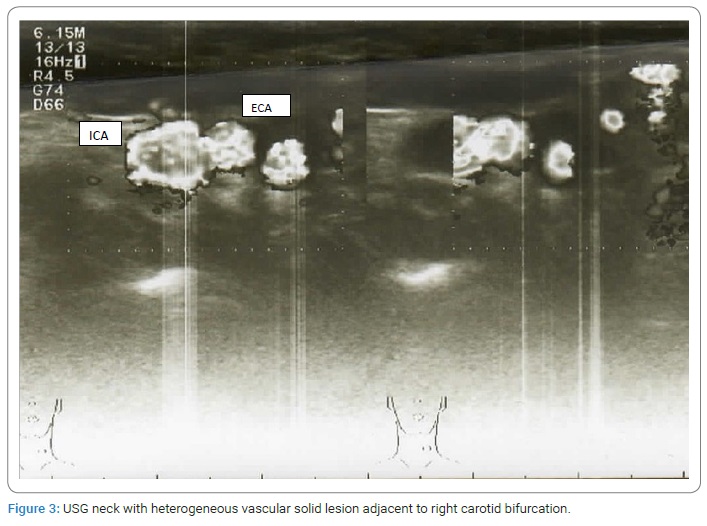
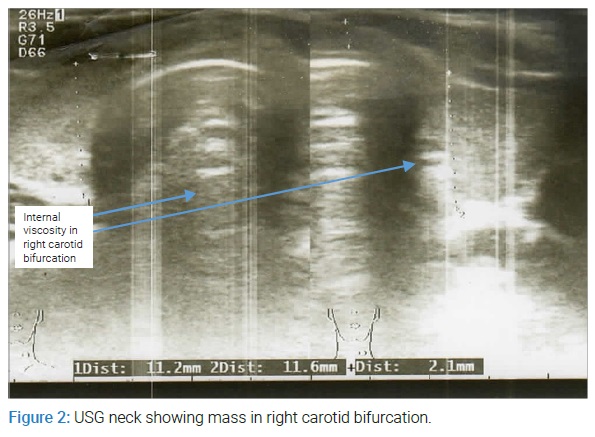
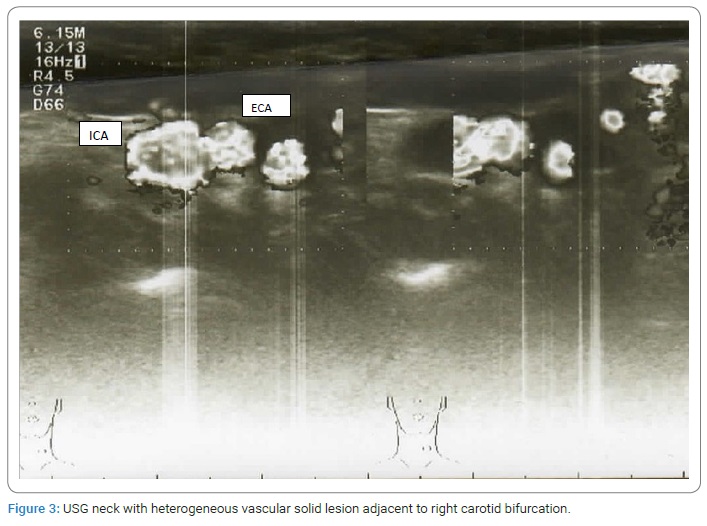
It was nonmobile with deglutition and no associated lymphadenopathy or discharge was noted. There was no similar history in the family. Following the examination findings, basic metabolic panel and hormonal studies were sent, which were in the normal range. Then, Ultrasonography (USG) of the neck was done which showed a well-defined heterogeneous vascular solid lesion adjacent to the right carotid bifurcation measuring about 18 mm X 17 mm. Internal viscosity was noted without calcifications and cystic components (Figure 2, Figure 3).
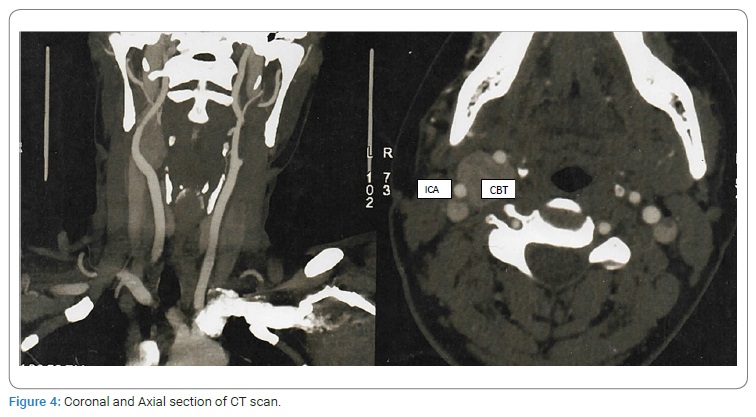
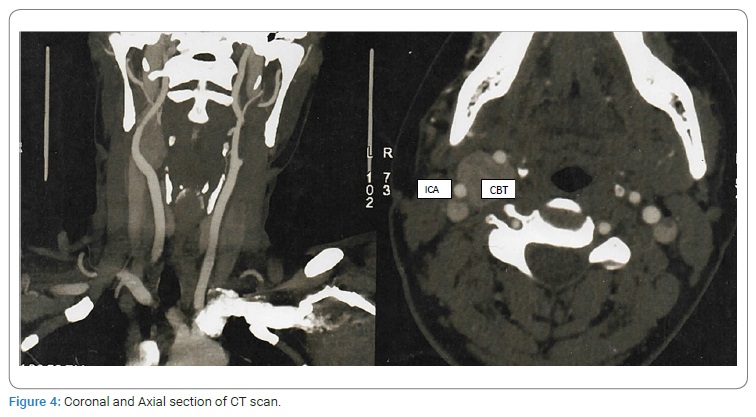
The USG of the abdomen and pelvis was normal. Subsequently, Contrast-Enhanced Computed Tomography (CECT) was done which demonstrated a markedly enhancing soft tissue density lesion measuring 32 mm X 20 mm X 18 mm in size, at the region of the right carotid bifurcation. The internal and external carotid arteries were partially encased by the tumor causing fraying of these arteries. No calcification was seen in the lesion. Another approximately 3 mm X 2 mm size small enhancing lesion was also noted in the left carotid bifurcation. All other structures of the neck were normal (Figure 4).
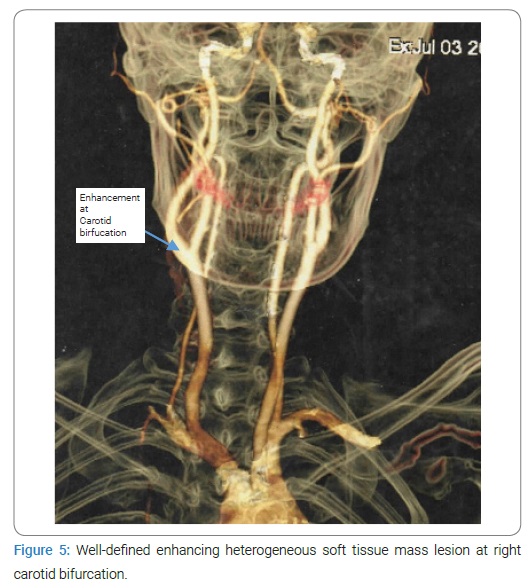
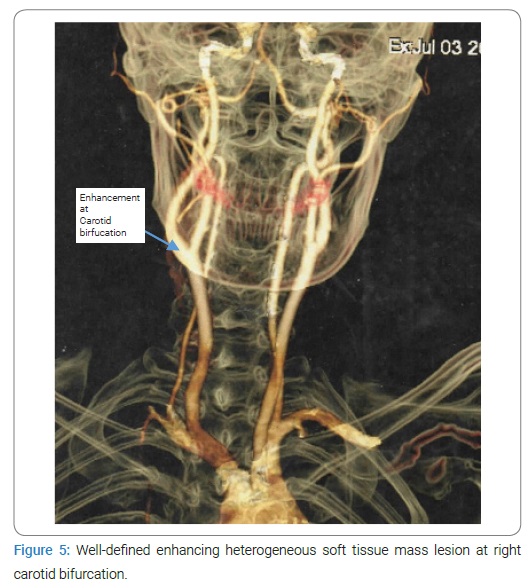
CT angiogram of the neck vessel which showed a well-defined avidly enhancing heterogeneous soft tissue mass lesion in the anterior triangle of the right neck at the carotid bifurcation with characteristic splaying of the right Internal Carotid Artery (ICA) and External Carotid Artery (ECA). It measured about 3.5 cm X 2 cm X 2 cm in Craniocaudal (CC), Transverse (TR) and Antero Posterior (AP) dimensions respectively. The lesion was perfused by the small twigs of the proximal right ICA. Partial encasement of the right ICA and ECA were also noted. Minimal indentation of the right internal jugular vein was noted with otherwise patent lumen. A tiny suspicious 3 mm X 2 mm sized enhancing lesion was noted in left carotid bifurcation (Figure 5, Figure 6).

Hence Carotid Body (CB) paraganglioma was suspected with the help of different imaging techniques. Then the tumor was excised under general anesthesia. The mass was completely removed and sent for histopathology. The patient was improved postoperatively and discharged on the third postoperative day. Excisional biopsy of mass at the right side of carotid bifurcation showed circumscribed mass with tumor cells arranged in an organoid pattern and separated by a prominent capillary network. Individual tumor cells were moderately pleomorphic, having abundant clear to light eosinophilic cytoplasm. The nuclei were round to oval with a vascular to granular chromatin pattern. Congested blood vessels, hemorrhage, and fibro collagenous were also noted. Two lymph nodes were identified that are negative for tumor cells.
Mitotic figures, necrosis, capsular and lymphovascular invasions were not seen. Excisional biopsy of carotid sheath showed thirteen lymph nodes with lymphoid follicles of variable sizes with a germinal center surrounded by mature lymphocytes. Sinus hyperplasia and congested blood vessels were also seen but no atypical tumor cell infiltration. The patient was followed up after 1 week. The wound was well healed and the patient has no further complaints (Figure 7).

Discussion
The CB was first described by Von Haller as a chemoreceptor located in the adventitia of carotid bifurcation. They are reddish-brown elliptical structures 5-7 mm X 2.5-4 mm that detect hypoxia, hypercarbia, and acidosis. The chemoreceptor carries these impulses via the vagus and glossopharyngeal nerves and plays a role in the autonomous control of blood pressure, heart rate, respiration, and body temperature by increasing sympathetic flow. Embryologically, the mesodermal component of the CB is derived from the second pharyngeal arch artery and the ectodermal component from the neural crest cell. CBT is a hypertrophic change that enlarges in response to hyperstimulation. CBT mostly predominates in the age group of 45–50 (range from 18 years–94 years), with high incidence in females. Bilateral disease is more frequently associated with familial cases compared to non-familial ones. CBTs are very slow-growing hypervascular tumors representing around 0.03% of all neoplasms. These tumors are reported more on the right side compared to the left. Around 10% of CBTs are malignant with local vascular and/or lymph node invasion and rarely metastasize to distant organs [2].
Notably, the lesion in the presented case is bilateral and doesn't have any malignant or neoplastic characteristics. CBT is usually painless, palpable, slow-growing, pulsatile round masses located anterior to sternocleidomastoid muscle at the angle of the mandible near the hyoid bone. If cranial nerves are involved, tumors can travel through the carotid sheath (Cranial nerve IX, X, XI, and XII). Symptoms are related to the nerves involved. Common symptoms include dysphagia, hoarseness, dysarthria, swallowing difficulties, and shoulder drop. The severity of these symptoms depends on the size of the tumor [3,4]. Other symptoms may include dizziness, headache, flushing, palpitations, tachycardia, arrhythmias, diaphoresis, and photophobia due to association with pheochromocytoma. However, the association with hypercatecholenemic state is not common. In a retrospective study of 25 CBT cases 84% were asymptomatic with a mean age of 49 years. The rate of stroke was 30% and cranial nerve injury was 32% over 30 days with a single case developing permanent nerve injury. Over the mean follow-up period of 1 year, there was no recurrence [4]. Even though CBTs are mostly asymptomatic and solitary, they can present along with other conditions. Neurological abnormalities are mostly presented with the compression of the cranial nerve 9 and 10. Horner's syndrome is also an unusual presentation in some patients. Benjamin and Wayne have presented a case report of bilateral CBT with 2 rare concomitant anatomic findings, an ectopic parathyroid gland and cervical thymus which might be because of their embryological origin [5]. Paragangliomas may be hereditary or sporadic. It may be part of genetic syndromes such as Von Hippel-Lindau syndrome, neurofibromatosis types I (von Recklinghausen disease), MEN 2A, and MEN 2B. So, the patients should be counseled about genetic testing as well, as they can help in the screening of other conditions associated with the syndromes. Zoe A has presented a case report on Cowden-like syndrome, neck paraganglioma, and pituitary adenoma. In the study, pituitary adenoma was argued to be interstellar paraganglioma that is so rare; only 6 cases reported to date [6]. Cowden syndrome, thyroid cancer, and carotid paraganglioma have similar gene mutations of PTEN and SDHD, which could be a rare coincidence as mentioned by some authors [7]. USG is the best initial test for neck masses where CBT appears as a hypoechoic mass in the carotid bifurcation with prominent vascularization. It helps to rule out the presence of lymph nodes, thyroid, or branchial cyst. Doppler can help in identifying the relationship of the tumor with the carotid sheath. CT and MRI help to identify the size, degree, and extension of tumors to adjacent regions [7,8]. Digital subtraction angiography used to be standard diagnostic imaging but nowadays, it is replaced widely by CT/MR angiography. In contrast-enhanced CT, CBT presents as a solid homogeneous enhancing mass. Sometimes, heterogeneous patterns can be demonstrated due to thrombosis or bleeding in the large tumor. CBT is rapidly enhanced whereas the carotid sheath is slowly enhanced due to its distance from the lumen. Lyre sign is seen in imaging which is due to displacement of ICA and ECA with splaying of the vessels [9]. Similarly, on T1-weighted images, CBTs are hypo to isointense compared to muscle and hyperintense on T-2 weighted images. "Salt and pepper" appearance is well demonstrated by lee KY and et al. The "salt" phenomenon is due to multiple punctuating hemorrhages inside the lesion, which presents as high signal intensity spots. The low signal intensity is due to multiple flow voids from intra-tumoral blood vessels giving a "pepper" appearance [10]. Treatment of CBT is mainly surgery. Preoperative embolization is commonly done to minimize blood loss, decrease the time to operate and the recurrence rate. However, it is not required for all CBTs. The decision to do embolization is made considering the size and vascularity of the tumor and surgeon preference [11]. There are three safe surgical modalities of treatment namely: Blunt Dissection (BD), BD plus resection of external carotid artery division plus vessels of encapsulation with allograft dermal matrix, and surgical resection of tumors plus common carotid artery-internal carotid artery artificial vascular reconstruction [12]. Although neoplastic CBTs are possible, histopathology is usually sent post-operatively. The metastatic sites included the lungs, bones, abdomen, and retroperitoneum. Malignant CBTs have advanced Shamblin classification and larger tumor size [13].Treatment of systemic spread of CBT is chemotherapy and radiotherapy [14,15].
Conclusions
Although neck mass presents most commonly with other conditions, Carotid Body Tumor (CBT) should also be kept in differentials. It can be diagnosed easily with imaging but also needs to be distinguished from malignant form. Surgical modality is most commonly done and follow-up is required for about a year.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Carotid body tumor; Neural crest cell; Lymph nodes; Hemorrhage; Carotid bifurcation
Cite this article
Prakash PJ, Jonas M, Kiran NP, Pratistha P, Bishal K, Kiran NS. A Case report on diagnosis and treatment of bilateral carotid body tumor. J Heart Disord. 2022;1(1):1–5.
Copyright
© 2022 Poudel Jaishi Prakash. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).