Abstract
The term “Refeeding syndrome” is defined by the immense changes in the electrolytes and fluid levels that could take place in the patients who are refeed artificially after suffering a long term malnourishment. An improved level of awareness as well as understanding of refeeding syndrome, with effectively managed strategy is important for nutritional rehabilitation of the individual. In this scenario, a gradual and deliberatesurge in nutritional intake with proper nutritional counseling, and psychotherapy are recommended by the experts. Our case study took a young 22 year-old girl suffering from anorexia with a BMI of 11.9. She had been misdiagnosed by the medical practitioner and got severe electrolyte imbalances in blood levels. This occurred only because ofthe lack of cognizance regarding refeeding syndrome. After the cautious clinical and nutritional assessment, empirical and scientific evaluation, different protocols can be suggested to prevent and manage this syndrome. Equally important is to instill awareness in the patient about refeeding slowly and building-up micronutrient gradually for several days in nutritional therapy.
Introduction
Refeeding Syndrome (RS) is possibly a serious condition, that is defined by severe fluid and electrolyte imbalances cause by damaging nutritional rehabilitation in patients who are conditioned to malnourishment [1]. The patients who are enduring protein energy malnutrition and severe weight loss are at a potential risk of developing RS in them. Those having condition such as anorexia nervosa and obesity are at high end risk [2]. Even though there are studies but the actual incidence of refeeding syndrome is still unknown to us. However a study on the topic of RS has demonstrated a prevelance rate of 0.45% in all of the hospitalized patients, where as malnutrition is one of the major risk factor [3]. The principal features of RS comprise severe hypophosphatemia, hypo-magnesia, and hypokalemia with other fluid imbalances and electrolyte abnormalities that could develop life-threatening irregularities in the central nervous system, cardiovascular system, including different pulmonary and hematologic complications [4]. Refeeding malnourished patients can emerge from “oral, enteral and parenteral nutrition” which in several cases could be life threatening for the patient if it goes undiagnosed and ill-treated.
The incident of a 22-year-old girl who had previously been suffering from the condition of anorexia nervosa is well known. She developed RS due an aggressive nutrition intake and was managed in a hospital with Total Parenteral Nutrition (TPN).
Case Report
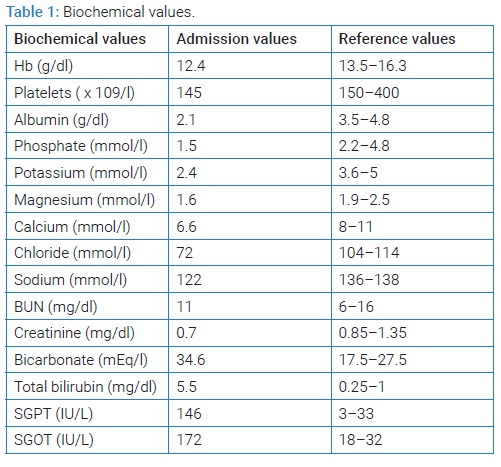
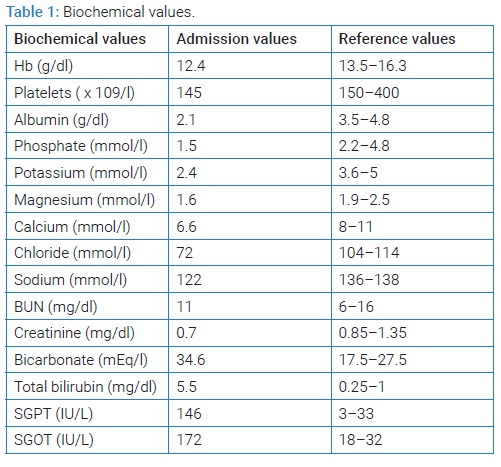
The 22-year-old girl living in Lahore had been admitted in the emergency care unit on September, 2021. She had a 2 days history of severe abdominal cramps, nausea and continuous vomiting. She endured the condition of secondary amenorrhea, and chronic constipation for two and half years before admission to the hospital. Not with standing, she had a psychiatric history of having anorexia nervosa, which is the fear of growing overweight and was on strict dieting schedule. The patient was asked to consume a large serving of meat just a day before her admission to hospital. She instantly developed fore-mentioned symptoms after eating the meal. Over the course fourteen weeks she lost eighteen kg of her weight. Upon examination, her weight was only twenty seven kilo grams and was 152 cm tall. As her Body Mass Index (BMI) stood at 11.9 which is extremely low. In addition to this her physical appearance was pale and weak. Her resting pulse rate was rapid (110 beats/minute), with a low blood pressure measuring just 90/40 mm/Hg. Upon her Chest and CVS examination nothing abnormal was found. However, the abdominal examination of the patient showed recessed abdomen with a moderate tenderness in her right iliac fossa and the visceral organs were not palpable. The laboratory tests of the girl revealed low albumin, hypophosphatemia, hypochloremic metabolic acidosis, hypokalemia. Her liver function tests showed a disturbed liver function (Table 1).
She had turn to several gynecologists during the last 2 years to consult secondary amenorrhea. She was recommended some medicines to regulate her monthly cycles, but her prolactin levels elevated later on. She was pre-occupied with the feelings of being overweight, despite the fact that her weight was only 42 kg with BMI of 18.6). The fear lead her to stop taking her medicines and she started dieting and vigor exercise. After wards she was taken for a psychiatrist consultation and there she was diagnosed with the condition of anorexia nervosa and was advised to take anti-depressants. In her case, no family psychiatric history was found and there was no major childhood illness. She was again presented to hospital 3 days later with stark phosphatemia, abdominal distension, feet swelling. There she was diagnosed with RS as her reports were claiming severe electrolyte imbalances. Then she was recommended for nutritional consultation was given TPN 1 (for precise intake). Later on her schedule was changed to TPN 2 as she was unable tolerate the oral intake. She had been prescribed a 1500 kcal/day diet plan and antiemetic before meals to stop nausea and vomit. She was also tied up into psychotherapy and motivational therapy. There was steady improvement in her condition and she was gradually substituted to a total oral consumption. In her 5th week of therapy, she added 6 kgs in her total weight. She was discharged from hospital with a prescription of esomeprazole, some antidepressants and other vitamin supplements.
Discussion
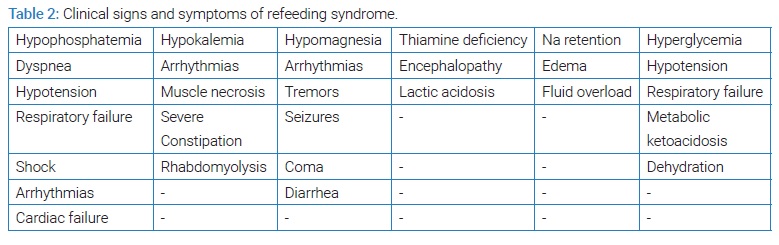
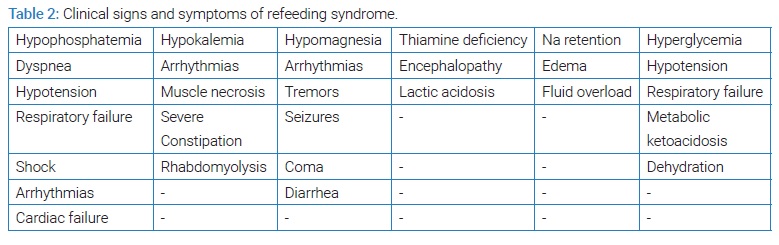
A forceful nutrient intake of carbs can evoke a release of insulin and increase levels of glucose, phosphate, magnesium etc in the blood. The severe electrolyte imbalances can end in severe complications including sudden death of the patients. Here, the natriuretic effect of insulin can cause sodium retention and oedema. Severe phosphatemia is the most prevailing feature of Refeeding Syndrome (RS) and can cause “dyspnea, respiratory failure, hypotension, shock, arrhythmias and cardiac failure”. The increase in the utilization of thiamine in such conditions can be resulted into thiamine deficiency in some of the patients, as indicated by the study of Wernicke's encephalopathy [5]. Other clinical symptoms are described in (Table 2).
A procedure for avoidance and controlling of RS specified the circumstances in which it is probably develop, and stressed the significance of refeeding gradually and compounding the micro nutritional content over few days with constant monitoring [4]. It highlighted that the administration should never be performed inhaste and the targeted weight accumulation should never surpass 1 kg to 1.5 kg per week.
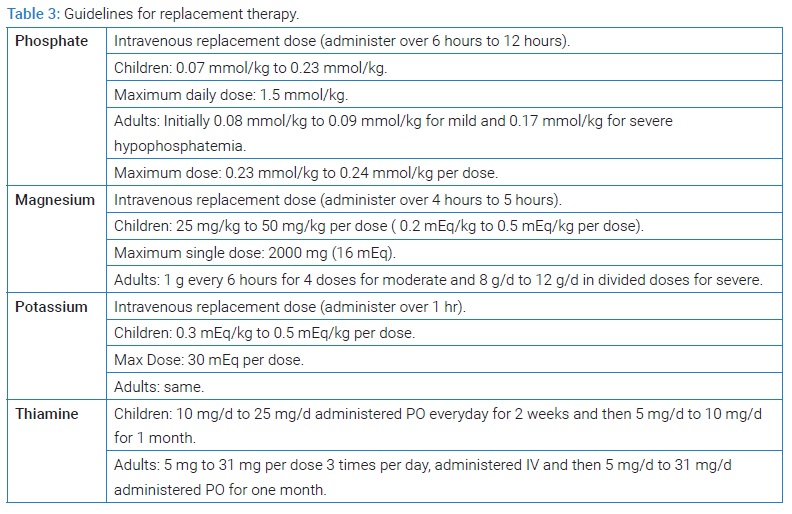
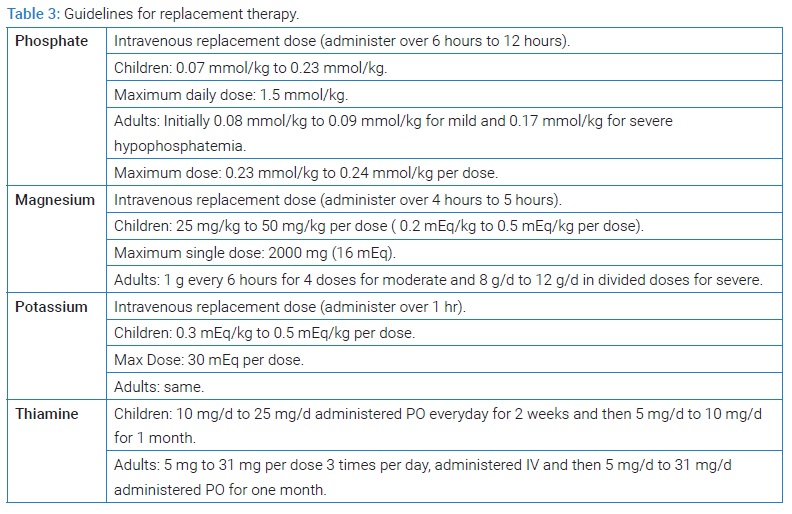
In the adults, studies suggested the starting the intake of 1000 kcal to 1200 kcal per day [6]. The protein intake must not be circumscribed during the nutritional provision [7]. The strategies for electrolyte and thiamine stabilization are given in (Table 3).
In conclusion, the‘nutritional rehabilitation’ is always a crucial element of the physical treatment of the disorders such as ‘anorexia nervosa’ and other conditions that may cause malnourishment. However, good psychological treatment is also of paramount importance in order to address the anxiety issues concerning the patient. Anupright therapeutic coalition between the doctor, patient and the family creates a collaboration that allows the work of motivational factors. The treatment at home is conferred in some studies is found to bear more benefits for the patients [1].
So, improved awareness and understanding of RS along with a well-coordinated plan are important in delivering safe and effective nutritional rehabilitation.
In summary, rehabilitation of anorexia nervosa or other starving states can result in fatal electrolyte disturbances (RS) and, therefore, proper and timely nutrition is recommended. We suggest a slow and gradual increase in nutrition along with nutritional counselling and psychotherapy, including the patient's family, to prevent resistance from the patient and to ensure long-term compliance by the patient.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Refeeding syndrome; Malnourishment; Anorexia nervosa; Nutritional rehabilitation
Cite this article
Khursheed T, Bashrat S, Jaffar M, Tahir H. Nutritional rehabilitation care of refeeding syndrome with anorexia nervosa. J Nutr Food Sci Metab. 2022;1(1):1–3.
Copyright
© 2022 Tara Khursheed. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).