Abstract
Familial Mediterranean Fever (FMF) is a hereditary auto inflammatory disease. Mutations of MEFV gene results in pyrin dysfunction, which causes uncontrolled interleukin-1 beta production and triggers the inflammatory attacks. Subclinical inflammation is still present even during attack-free periods in one-third of the FMF patients.
Strong evidences from basic research and clinical epidemiological studies have shown increased early markers of endothelial dysfunction, and hypercoagulable state in FMF patients due to the recurrent/chronic inflammatory of this disease.
Herein, we present a 9-year-old girl, followed for FMF disease with homozygous mutation on M694V since five years. She experienced a bilateral thalamic infraction. An exhaustive etiological assessment came back negative. Therefore the relationship between this cerebrovascular accident and FMF is plausible.
Introduction
Familial Mediterranean Fever (FMF) is prevalent in specific ethnic groups, namely, non-Ashkenazi Jews, Armenians, Turks and Arabs. FMF is a monogenic hereditary disorder, whose gene causing (Me FV gene) was identified in 1997. It is characterized by recurrent episodes of fever in the course of serosal, synovial, or cutaneous inflammation [1]. The flares of the disease are followed by asymptomatic periods during which it is believed that subclinical inflammation is still present. This condition, of low-grade inflammation, could favor endothelial dysfunction and atherosclerosis. This chronic inflammatory process affects both large and small blood vessels [2]. FMF was also associated with a hypercoagulable state even in attack free, sub-clinically inflamed patents [1–3].
Here in we present a rare case of cerebrovascular accident in 9-year-old girl with FMF.
Case Report
A young 9-year-old girl, who was born to a consanguineous marriage, followed for FMF with homozygous mutation on M694V since 5 years, receiving colchicine therapy irregularly. Show as admitted for sudden onset of behavioral disorder with agnosia that had begun 7 days before. Two months earlier, she started anti tuberculosis treatment for peritoneal tuberculosis which was confirmed by the anatomopathologic study. It was noted that the immune assessment was normal with a negative HIV serology.
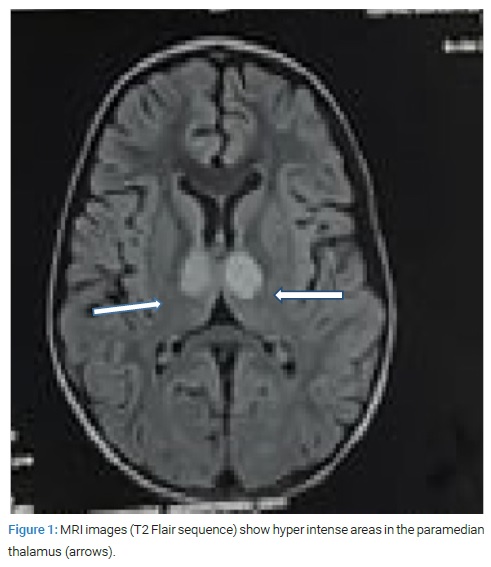
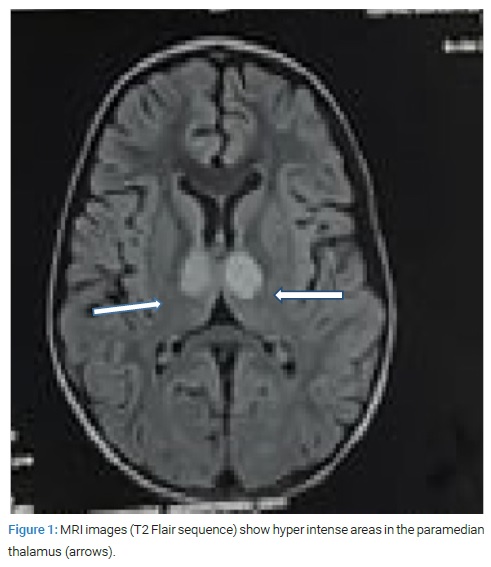
At the admission, the vital signs were stable. Chest and abdominal examinations were normal. She had no localizing signs or involvement of the cranial nerves. A complete blood count was obtained, which showed a normal white cell count and differential, a normal platelet count. Serum electrolytes, glucose level, liver function tests, creatine phosphokinase and partial thromboplastin time were all normal. She had an erythrocyte sedimentation rate of 45 mm/h and a C reactive protein of 20 mg/L. A brain Magnetic Resonance Imaging (MRI) revealed evidence of bilateral thalamic infarction due to occlusion of the percheron artery (Figure 1).
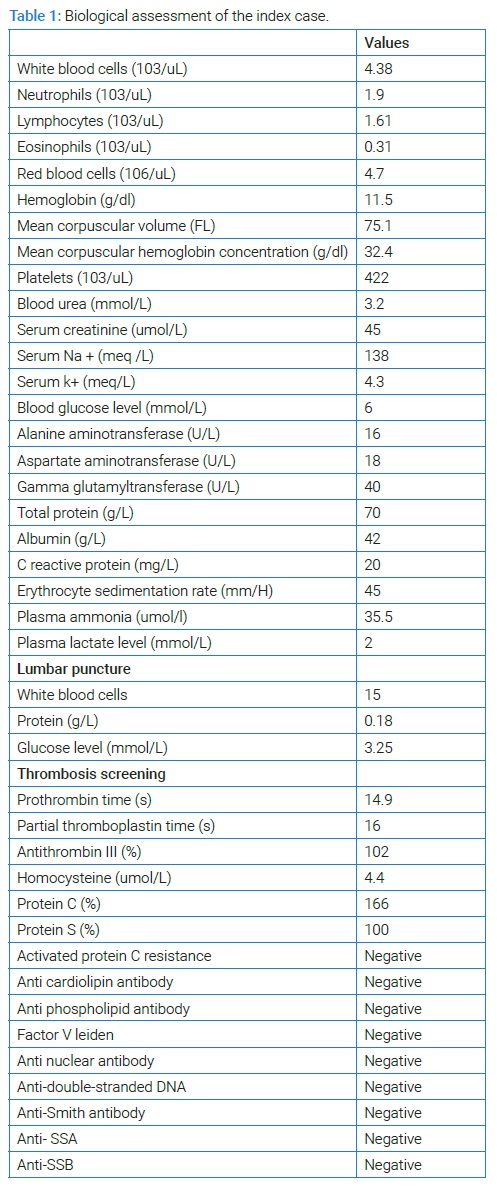
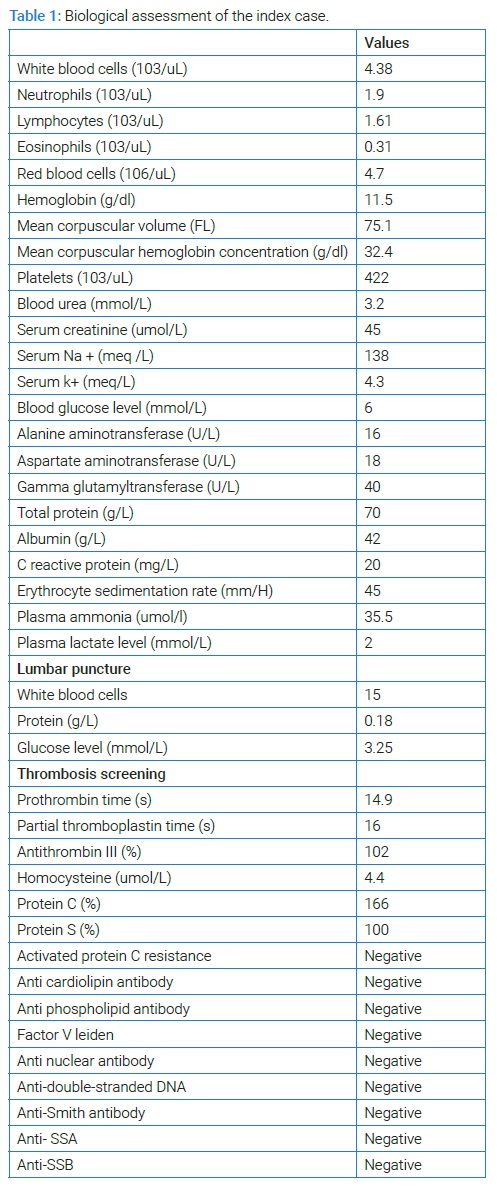
She underwent a series of tests to determine the etiology of this stroke. An echo cardiography was obtained, and a lumbar puncture was done to eliminate neuromeningeal tuberculosis, being both normal. Serum levels of protein C, protein S, anti thrombin III, homocysteine, and anticardiolipin Ab (IgG) were in normal range and there is no resistance to activated protein C.Factor V Leiden test was also negative. Vascular markers including Anti Nuclear Antibody (ANA), anti-Double-Stranded DNA (anti-DSDNA), anti-Smith antibody (anti-SmAb), anti SSA et SSB anti bodies were negative (Table 1). Metabolic diseases suggestive of Leigh's syndrome have been ruled out. She was discharged after two weeks of admission with prescription of valproic acid, vitamin E, colchicines and anti tuberculosis treatment. No new neurologic complaints or remaining complication from previous attacks was found on the follow-up visit.
Discussion
Familial Mediterranean fever is an autosomal recessive disease manifested by inflammatory attacks of peritonitis, pleuritis, pericarditis accompanied by fever and arthritis [1–3]. Neurological manifestations of FMF occur rarely and included myelinating (MS-like) lesions, posterior reversible encephalopathy syndrome, and pseudo tumor cerebri [1,4].
However, the association between FMF and cerebral stroke is a rare finding that has not been studied yet thoroughly and is limited to a report of four cases and two retrospective studies. One case report about a 13-year-old Palestinian girl who in addition to FMF had several prothrombotic defects, which actually seemed to be the culprit, rather than the FMF [3], the second about a 21-year-old man with nephritic syndrome complicated by AA amyloidosis, and lupus anticoagulant in low titre, the third and the fourth cases about two young male patients who suffered of a brain stem infarction during a typical FMF attack [1,5].
The retrospective study by Kalyoncu et al. in 2010, identified seven cases of stroke among 3034 FMF patients. The mean age was about 28.5 years. Vertebrobasilar vessels were the most affected and six patients were homozygous for the M694Vmutations. Three of them had also established risk factors for stroke, such as hemodynamically significant patent foramen ovale, thalassemia major and carotid artery dissection [6]. We notice that MEFV mutation (M694V) was significantly over represented in cohorts infarcted patients [6,7].
Feld et al. [6] reported a diagnosis of stroke/transient ischemic attack in 11 FMF patients younger than 50 years, admitted to Sheba Medical Center from 1985 to 2010. In this study, other risk factors prevailed: two of the stroke patients had renal amyloidosis and were on hemodialysis, and three had at least one risk factor for stroke including smoking, hypertension, diabetes mellitus and obesity.
The present case was 9-year-old and carrier of the MEVF mutation (M694V). She had a bilateral thalamic infarction due to occlusion of the percher on artery and she has been undergoing treatment for peritoneal tuberculosis since two months. The etiological assessment was negative, and there are no studies that have reported a relationship between anti tuberculosis treatment and ischemic stroke. Thus, the occurrence of stroke in the current case with a young age and without any possible explanation other than underlying FMF seems rational.
Studies have shown increased early markers of endothelial dysfunction, atherosclerosis and hypercoagulable state in FMF patients, suggesting an increased stroke rate [3,8].
Indeed, inflammation is a well-known prothrombotic condition and FMF is no exception [1,2]. Mutations of MEFV gene lead to pyrin dysfunction, which causes uncontrolled IL-1β production to trigger the inflammatory attacks [1,8]. Several other measurements of pro-inflammatory cytokines such as IL-6, IL-8, IL-12, IL-17 and IL-18 in the serum of FMF patients, either with or without acute attack, revealed a significant elevation of both cytokines compared to healthy controls [5–8]. Rapid increases of pro-inflammatory cytokine patterns were seen during attacks and high levels may persist during free interval. That indicates a continuous subclinical disease activity and inflammation that can induce endothelial dysfunction in FMF [1,2].
Other inflammatory markers, such as homocysteine, fibrinogen, lipoproteina and Plasminogen Activator Inhibitor 1 (PAI-1) (which are risk factors for atherosclerosis), were all been found to be statistically significantly elevated in FMF patients compared to healthy individuals [2].
In other recent studies, mean platelet volume, a new risk factor for atherothrombosis, was found to be higher in FMF patients compared to healthy controls [2].
Many studies confirmed the presence of endothelial dysfunction in FMF patients comparatively to healthy controls. They showed an arterial stiffness by studying Pulse Wave Velocity (PWV) and an increased in time-media thickness of the carotidartery accompanied by other markers of enhanced atherosclerosis [2–8].
The present case was receiving colchicine treatment irregularly. Similarly, the various ischemic vascular events have been reported in patients who started colchicine late or those with poor treatment compliance [6,8]. These facts confirm the anti-inflammatory and antithrombotic effect of clochicine [2]. Indeed, a controlled study showed a normal prevalence of overt cardiovascular disease in FMF and the important limitation of this study was the treatment with colchicine [6]. In case of resistance or intolerance to colchicine, IL-1 antagonists and anti-TNFs are recommended [8].
Conclusion
The various studies have demonstrated a concomitant activation of the inflammation and the coagulation cascade in patients with Familial Mediterranean Fever (FMF), which leads to a higher prevalence of thrombotic manifestations. Keeping the rare presentation of FMF can avoid delayed diagnosis. Regular and early therapy with colchicine can preclude serious complications.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Familial mediterranean fever; Cerebrovascular accident; Colchicine
Cite this article
Haddad S, Amdouni R, Mezghani F, Jebebli E, Rhayem S, Fdhila F, et al. Familial mediterranean fever rare cause of cerebrovascular accident. Glob J Pedia. 2022;1(1):1–4.
Copyright
© 2022 Haddad Samir. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).