Interaction of Age and Comorbidities in the Risk of COVID-19 Mortality in New York City
* Victor M. Cardenas;
Robert R. Delongchamp;
-
* Victor M. Cardenas: Department of Epidemiology, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, Arkansas 72205, United States.
-
Robert R. Delongchamp: Department of Epidemiology, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, Arkansas 72205, United States.
-
May 25, 2022 |
-
Volume: 1 |
-
Issue: 1 |
-
Views: 1255 |
-
Downloads: 1090 |
Abstract
Objectives: To assess the Separate and joint effect of age and any chronic diseases or obesity on the risk of COVID-19 mortality.
Methods: We used publicly available data from New York City, Department of Health and Mental Health on COVID-19 mortality counts as of September 11, 2021, among adults by age and presence of any chronic disease or obesity. Prevalence estimates by age and presence of any chronic disease or obesity were obtained from the Behavioral Risk Factor Surveillance system for the New York-Jersey City-White Plains, NY-NJ, Metropolitan Division. These prevalence estimates were applied to the population of adult residents of the City as an estimate of the at-risk population. We calculated mortality risk ratios and their 95% confidence intervals using Poisson regression and the relative excess risk due to interaction and synergy factor.
Results: The mortality risk ratio for persons 65 and older with chronic conditions or obesity was greater than individual effects of being 65+ years of age or having the chronic conditions alone. There was evidence of a strong interaction of age and those conditions in the additive scale (relative excess risk due to interaction = 484.5 [95% CI = 404.2, 586.7], and a synergy factor of 5.0 (95% CI = 3.0, 8.5). Almost two-thirds (65.6%) (Population attributable proportion for additive interaction [95% CI: 56.8%, 72.6%]) of the COVID-19 mortality in NYC in 2020–2021 was due to the interaction of older age and chronic disease/obesity.
Conclusions: Presence of chronic conditions or obesity among those 65 years of age and older increased the risk of mortality above either old age or chronic disease alone.
Introduction
The risk of mortality from COVID-19 increases with age and the presence of underlying medical conditions. From the start of the pandemic in Wuhan, China, it was noted that 57% of severe/fatal cases had 1+ major chronic disease [1,2]. A report based on 1,482 hospitalized COVID-19 cases in 99 counties in 14 US states during March 2020, indicates that among 178 patients with data on underlying medical conditions, 89% had chronic conditions, including: hypertension (49.7%), obesity (48.3%), chronic lung disease (34.6%), diabetes mellitus (28.3%), and cardiovascular disease (27.8%) [3]. Another case series study based on 5,700 COVID-19 admitted patients in the New York City (NYC) area, 88% had more than one comorbidity, and suggested that hypertensives and diabetics had 2.5 and 2.0-fold risk of death [4]. Similarly, a report on 1,590 COVID-19 admissions recorded from 575 hospitals across China, at least 90% of them from Hubei Province, indicates that having 2+ comorbidities increased the fatality by a factor of 4.9 (95% CI: 3.2, 7.6) [5]. One of the first reports of the Chinese CDC provided mortality figures for persons with cancer, chronic lung disease, hypertension, diabetes, and cardiovascular disease that were 8 times to 9 times the rates of persons without any of those conditions, even though information on comorbidities were missing for 53.0% of the cases, and 60.3% of the deaths [2]. A report on hospital admission and mortality from COVID-19 based on the examination of records of > 26 million beneficiaries of the Medicare program, which by eligibility is limited to persons 65+ years of age, did not examine the effect of older age and chronic disease separately and jointly, but rather addressed the issue of confounding by controlling the effect of comorbidities by age [6]. Similarly, a recent systematic review and meta-analysis of the effect of obesity and obesity related health conditions on COVID-19 mortality did not address the issue of effect modification [7]. In actuality most cohort studies examined are large case series of COVID-19 patients.
Surprisingly, no previous study has related the occurrence of fatal COVID-19 cases to the population at-risk, one of the basic principles of epidemiology. We used the New York City, Department of Health and Mental Hygiene (NYC DoH & MH) publicly available data on age and chronic conditions for deaths recorded as due to COVID-19 and estimates of prevalence of those conditions by age among residents of New York City, to assess the role of age and comorbidities on the mortality risk from COVID-19 in the ongoing pandemic.
Methods
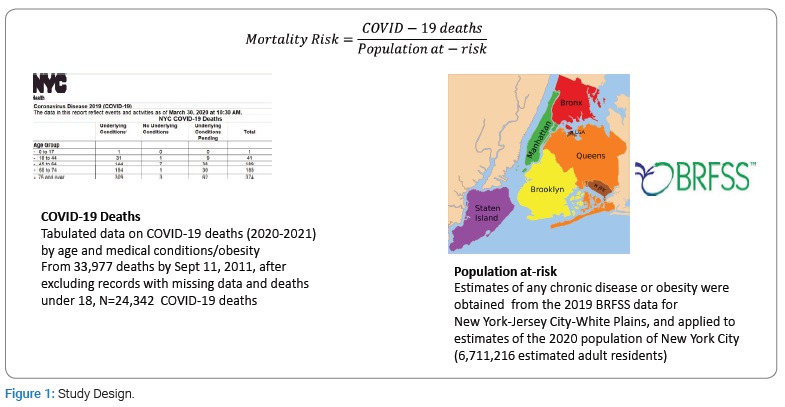
The (Figure 1) depicts design of this ecological study using public health surveillance data. Early on during the pandemic, the NYC DoH & MH started publishing daily updates on the presence of diabetes, lung disease, cancer, immunodeficiency, heart disease, hypertension, asthma, kidney disease, GI/liver disease among COVID-19 decedents among residents of the City. NYC DoH & MH added obesity to the list in mid-April 2020. We used these data as of September 11, 2021, as numerator data for mortality risk analysis (Supplemental file). To compute the at-risk population, that is the denominator, we applied to the population estimates of the Department of City Planning of the City of New York by age for 2020 [8], estimates of the prevalence of those conditions derived from the 2017 Selected Metropolitan/Micropolitan Area Risk Trends (SMART) project that uses the Centers for Disease Control and Prevention (CDC) Behavioral Risk Factor Surveillance System (BRFSS) for the Metropolitan area of New York-Jersey City-White Plains, NY-NJ, Metropolitan Division (MMSA code: 35614). These estimates were considered the closest available estimate of prevalence of those conditions applicable to the actual study population. The data released for 2019 was selected because it had data on high blood pressure. We obtained weighted estimates of the prevalence of a combination of self-report of any of the following medically diagnosed conditions: chronic obstructive pulmonary disease, asthma, diabetes, hypertension, kidney disease, heart disease, cardiovascular disease, cancer (other than non-malignant melanoma skin cancer) and obesity (body mass index ≥ 30) (n = 4,152 participants of the 2019 SMART in the study population). There was no data on immunodeficiency or GI/liver disease.
We obtained prevalence estimates of those chronic conditions and obesity using SUDAAN (version 11, RTI, NC). Risk (synonymous cumulative incidence, incidence proportion or attack rate) is defined as “the probability of an adverse or beneficial event in a defined population over a specified time interval” [9]. We calculated a mortality risk by dividing the reported deaths from COVID-19 by our estimate of the population at risk.
We then compared the risk of mortality by age and chronic conditions risk using Mortality Risk Ratios (MRR). We used Poisson regression analysis to assess effect modification and confounding by age and medical conditions/obesity with SAS (SAS 9.4, Cary, NC) PROC GENMOD. The Relative Excess Risk due to Interaction (RERI), the Attributable Proportion (AP) due to interaction and Population Attributable Risk (PAR) percent and their 95% confidence interval estimated using methods described elsewhere [10,11]. We also computed the synergy factor, a measure of interaction on the multiplicative scale, and its 95% confidence interval with estimators presented elsewhere [12].
Results
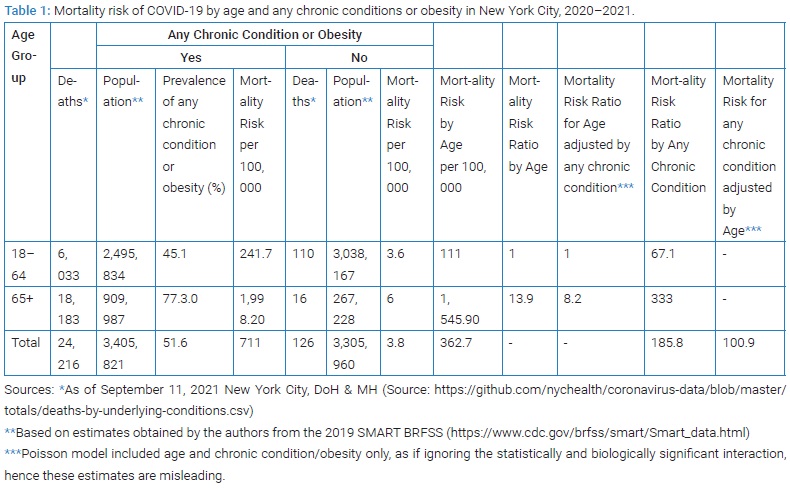
NYCDOH & MH reported 33,977 deaths with COVID-19 as the underlying cause of death by September 11, 2021. Only 29 COVID-19 deaths occurred in persons < 18 years of age, and data on age was missing in additional 28 instances. Among the remaining 33,920 deaths, their status regarding underlying medical conditions and obesity was pending for 9,578 (28.2%), leaving 24,342 informative events. In 24,216/24,342 (99.5%) of COVID-19 deaths in adults, at least one underlying medical condition or obesity was noted. The corresponding proportion among New York City, adults who reportedly had those medical conditions or obesity in 2019 was estimated at 51.6% (95% CI 47.0%, 56.1%). The age-specific prevalence of any of those chronic conditions or obesity was 1.7 times as large among 65+ years of age (77.3%) than among those in the 18 years to 64 years of age (45.1%). The COVID-19 mortality risk among 65+ year-olds were 13.9-times the risk of 18 years to 64-year-old (Table 1). The COVID-19 mortality rate among those with any chronic conditions or obesitywere183.9-times those of persons without chronic conditions or obesity (Table 1).
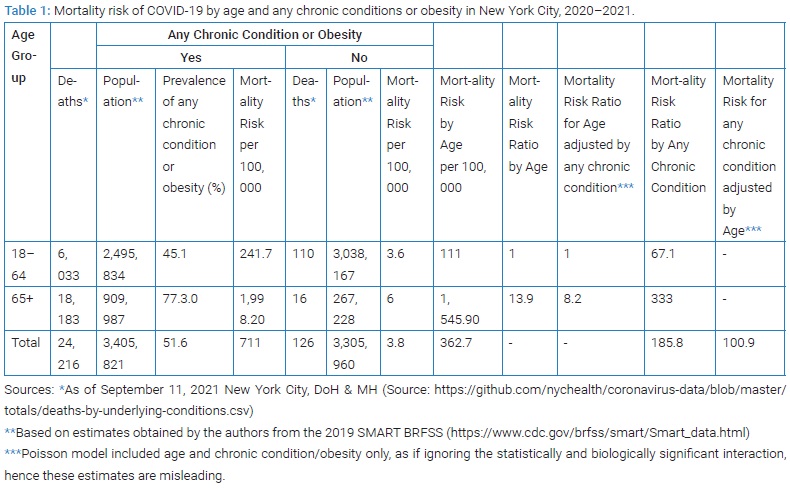
Using a Poisson regression model that included age and chronic disease/obesity, the COVID-19 mortality rate was 100.9 times for those with any underlying chronic condition or obesity (95% CI: 84.7, 120.3) compared to those without such conditions, while the mortality rate for ages 65+ year-olds were 8.2 (95% CI: 8.0, 8.4) times the risk of those in the 18 years to 64 years bracket. Thus, the effect of older age (65+) in a multivariate analysis decreased by 41%([13.9−8.2]/13.9) once adjusted for any chronic disease/obesity. In turn, the effect of any chronic condition or obesity also decreased by 45% ([183.9−100.9]/183.9), indicating there was mutual positive confounding of both variables.
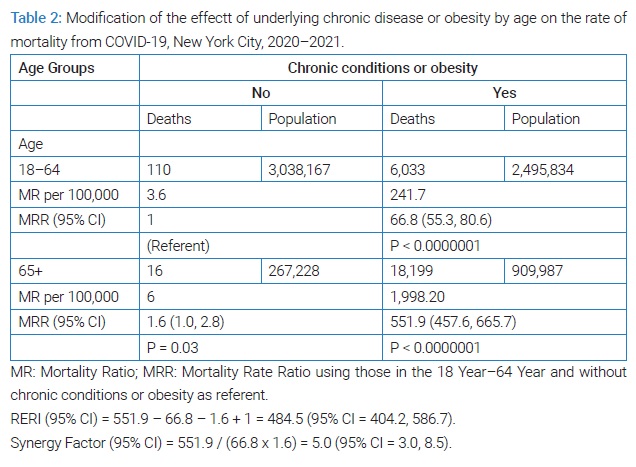
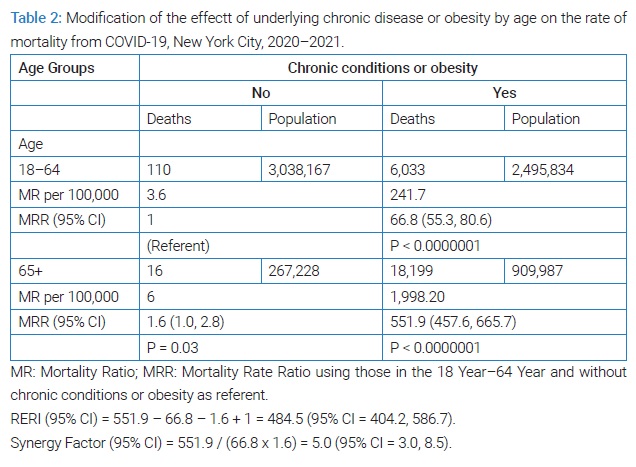
However, the following analysis suggested that the joint effects of age and comorbidities took over the interest of confounding as shown in (Table 2). The MRR among 65+ year old with underlying chronic conditions or obesity was 551.9 (95% CI: 457.6, 665.7), using the death risk of 18 to 64 without any of those conditions or obesity as referent. This effect was more than the expected from the independent effects of age 65+ without chronic diseases or obesity (MRR: 1.6; 95% CI: 1.0, 2.8), which was borderline significantly different from 1, or the effect of chronic disease or obesity alone in the 18 years to 44-year-old (MRR: 66.8; 95% CI: 55.3, 80.6) on COVID-19 mortality. The interaction term of pre-existing chronic conditions/obesity and age 65+ years of age was statistically significant when entered in a Poisson regression model (P < 0.001). The measure of Excess Risk due to Interaction (RERI) indicated a strong departure from additivity: RERI = 484.5 (95% CI: 404.2, 586.7), the AP was 87.8% (95% CI: 87.4%, 88.2%) and the PAR was 65.6% (56.8%, 72.6%). There was also a departure from the multiplicative scale, the synergy factor was 5.0 (95% CI: 3.0, 8.5).
Discussion
Our findings provide a quantitative assessment of key risk factors for chronic disease such as obesity, diabetes and high blood pressure, and chronic disease itself on the risk of mortality from COVID-19, and the assessment on how the presence of chronic diseases act synergistically with increasing age.
Since the joint effects of age and chronic conditions largely exceeds the sum of the single effects of each factor, suggest that assigning higher priority to suspect patients with both conditions could result in greater impact of efforts to reduce COVID-19 mortality.
Our analysis has significant limitations including the self-reported nature of medically diagnosed conditions in BRFSS, the lack of data on HIV or GI/liver disease status, and the large proportion (16%) of NYC deaths with pending status regarding those conditions. In addition, recorded deaths with COVID-19 as underlying cause of death, maybe more representative of those occurring in facilities, missing some ‘excess deaths’ more likely to occurred in nursing facilities or at home, but the latter may not have data on chronic disease or obesity. By some accounts, as many as other 5,000 deaths were missed. It is possible that the ascertainment of the contributing causes in death certificates by the NYC DoH & MH staff during the early waves of the pandemic in the USA will never be replicated: indeed, since September 11, 2021, no more records on this public file have been released. Our denominator does not exactly match the population living within the boroughs of NYC. In addition, the data on deaths did not include prognostic factors or other potential confounders. However, one has to keep in mind that the primary purpose of such data was to provide data on one of the multiple sources of public health surveillance data used to monitor the trends of mortality at the time the pandemic struck that community. The NYC DoH & MH set a standard of data collection and monitoring on comorbidities.
Future studies need to evaluate the contribution of each chronic condition, and obesity, and tease out race/ethnicity disparities in COVID-19 mortality [13]. The mechanism by which chronic conditions increase mortality from COVID-19 has not been determined. It could relate to impaired immunity as suggested by a recent prospective study of participants of the National Health and Nutrition Examination Survey, which reported an association between low count of lymphocytes and increased mortality [14]. The relation between plasma viscosity and hyperfibrinogenemia, a finding in some of the COVID-19 patients, and age and comorbidities [15], and chronic inflammation observed in chronic diseases deserve the inquiry as well [16]. Examination of excess COVID-19 mortality among centenarians led to speculate that a protective cohort effect among those born before the 1918 to 1919 influenza A pandemic [17]. The tabulation of the NYC DoH & MH data on the public domain by age groups does not allow us to examine this conjecture but this issue could possibly be addressed by future studies.
Public Health Significance
Our analysis suggests that providers should pay more attention to the presence of chronic conditions including obesity as background of COVID-19 patients particularly in older patients.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX. Clinical Characteristics of Coronavirus Disease 2019 in China. Engl J Med. 2020;58(4):711–712.
- Epidemiology working group for ncip epidemic response, chinese center for disease control and prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 2020;41(2):145–151.
- Garg S, Kim L, Whitaker M, O’Halloran A, Cummings C, Holstein R, et al. Hospitalization rates and characteristics of patients hospitalized with laboratory-confirmed Coronavirus disease 2019 — COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(15):458–464.
- Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA. 2020;323(20):2052–2059.
- Guan WJ, Liang WH, Zhao Y, Liang HR, Chen ZS, Li YM, et al. Comorbidity and its impact on 1590 patients with COVID-19 in China: a nationwide analysis. Eur Respir J. 2020;55(5):2000547.
- Izurieta HS, Graham DJ, Jiao Y, Hu M, Lu Y, Wu Y, et al. Natural history of Coronavirus disease 2019: risk factors for hospitalizations and deaths among > 26 million us medicare beneficiaries. J Infect Dis. 2021;223(6):945–956.
- Poly TN, Islam MM, Yang HC, Lin MC, Jian WS, Hsu MS, et al. Obesity and mortality among patients diagnosed with COVID-19: a systematic review and meta-analysis. Front Med. 2021;8:620044.
- City of New York, Department of City Planning. New York city population projections by age/sex & borough, 2010–2040. 2013. https://www1.nyc.gov/assets/planning/download/pdf/planning-level/nyc-population/projections_briefing_booklet_2010_2040.pdf. Accessed May 12, 2022.
- Porta M. A Dictionary of Epidemiology. 6th ed. New York: Oxford University Press; 2016.
- Rothman, KJ, Greenland S, Lash TL. Modern epidemiology. 3rd Edition. Philadelphia PA: Wolters Kluwer/Lippincott Williams & Wilkins. 2008.
- Zou GY. On the estimation of additive interaction by use of the four-by-two table and beyond. Am J Epidemiol. 2008;168(2):212–224.
- Cortina-Borja M, Smith AD, Combarros O, Lehmann DJ. The synergy factor: a statistic to measure interactions in complex diseases. BMC Res Notes. 2009;2:105.
- Laurencin CT, McClinton A. The COVID-19 Pandemic: a Call to Action to Identify and Address Racial and Ethnic Disparities. J Racial Ethn Health Disparities. 2020;7(3):398–402.
- Zidar DA, Al-Kindi SG, Liu Y, Krieger NI, Perzynski AT, Osnard M, et al. Association of Lymphopenia with risk of mortality among adults in the US general population. JAMA Netw Open. 2019;2(12):e1916526.
- Maier CL, Truong AD, Auld SC, Polly DM, Tanksley CL, Duncan A. COVID-19-associated hyperviscosity: a link between inflammation and thrombophilia? Lancet. 2020; 395(10239):1758–1759.
- Cohen S, Janicki-Deverts D, Doyle WJ, Miller GE, Frank E, Rabin BS, et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci U S A. 2012;109(16):5995–5999.
- Poulain M, Chambre D, Pes GM. Centenarians exposed to the Spanish flu in their early life better survived to COVID-19. Aging. 2021;13(18):21855–21865.
Keywords
Comorbidities; Public health; COVID-19; Chronic diseases; Mortality
Cite this article
Cardenas VM, Delongchamp RR. Interaction of age and comorbidities in the risk of COVID-19 mortality in New York City. World J Public Health Epidemiol. 2022;1(1):1–5.
Copyright
© 2022 Victor M. Cardenas. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).