Abstract
A rare congenital disease called Mounier Khun Syndrome was described in 1932. It is characterized by recurrent lung infections and dilatation of the trachea and main bronchi. The symptomatology is variable ranging from a simple lower respiratory infection or even the death of the patient. Thoracic computed tomography is the key examination for the diagnosis of this disease. Our patient is a 70-year-old man who had been presented for recurrent lung infections and was diagnosed with Mounier Kuhn syndrome or tracheobronchomegaly. In a low-resource country like Madagascar, diagnosing this rare disease is difficult, hence the objective of presenting this clinical case.
Introduction
A rare congenital disease was described in 1932 by Mounier Kuhn and was named Mounier Kuhn Syndrome. A defect in the cartilaginous rings of the tracheobronchial tree causes marked dilation of the trachea and main bronchi, which is the hallmark of this disease, leading to recurrent lower respiratory tract infections [1,2]. The etiologic mechanism remains unknown although cigarette smoke and air pollutants may act as irritants. Connective tissue diseases such as Ehlers-Danlos syndrome, Marfan syndrome and cutis laxa can be associated with this condition, the genetic origin of which is not yet known [3].
Presentation of the Patient
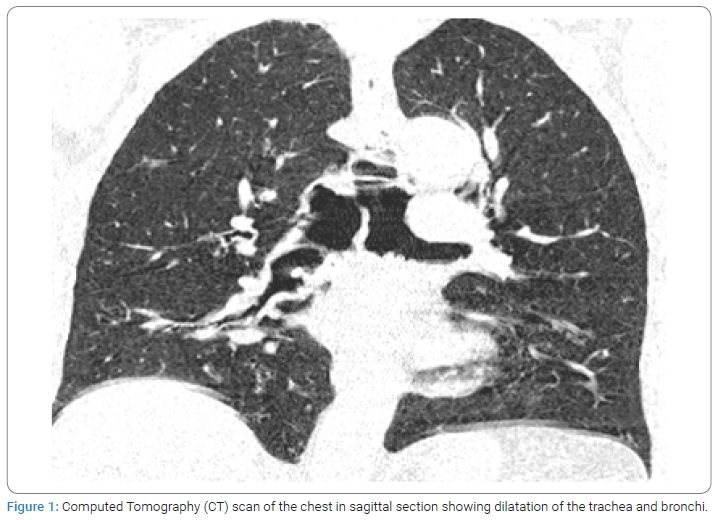
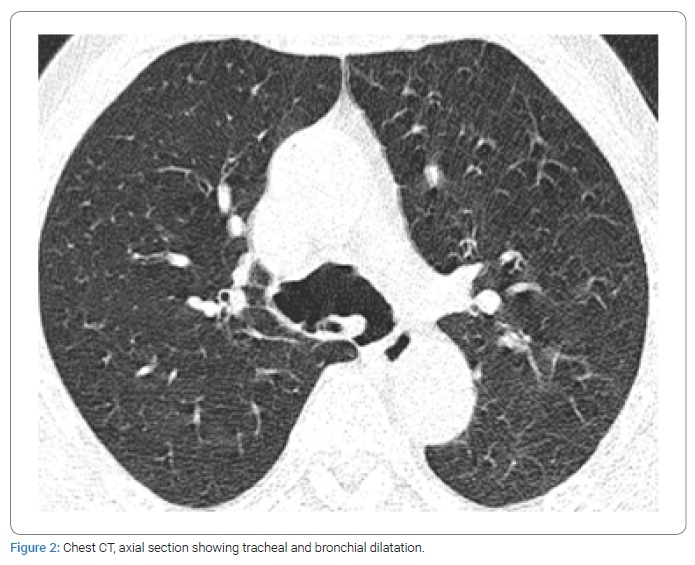
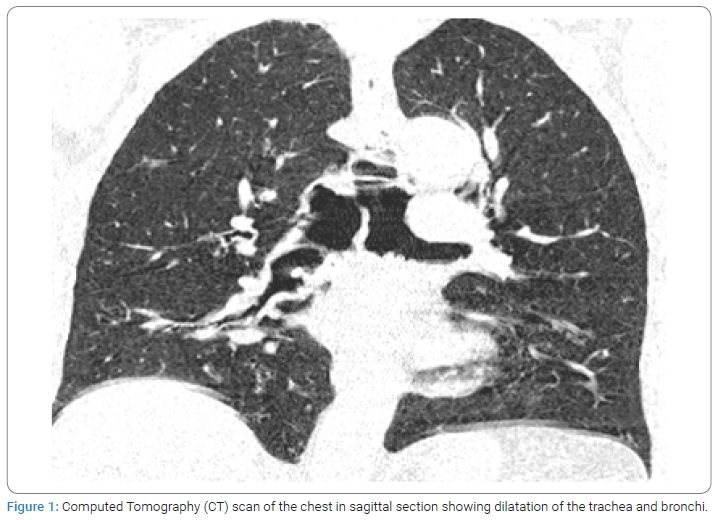
Mr R, a 70-year-old patient, a 15-year smoker, grade II hypertensive, stable and Chronic Obstructive Pulmonary Disease (COPD) known for 10 years and having a history of recurrent respiratory infections but no family history of congenital, pulmonary or infectious diseases. He came to an outpatient pneumological consultation for chronic cough with whitish expectoration evolving in an apyretic context. The clinical examination found a hemodynamically stable patient with bilateral ptosis, digital clubbing and diffuse sibilant rales on pulmonary auscultation. Biological examinations had found nothing special apart from polyclonal hypergammaglobulinemia. Spirometry revealed a 42% amputation of vital capacity, a drop in FEV1 to 47%, a FEV1/FVC ratio to 63%, a collapse in peak flow to 37% and distal airflows with an obstructive ventilatory disorder. Thoracic computed tomography showed dilatation of the trachea measuring 39 mm in diameter (Figure 1), and dilatation of the thin-walled bronchi presenting multiple parietal diverticula (Figure 2).
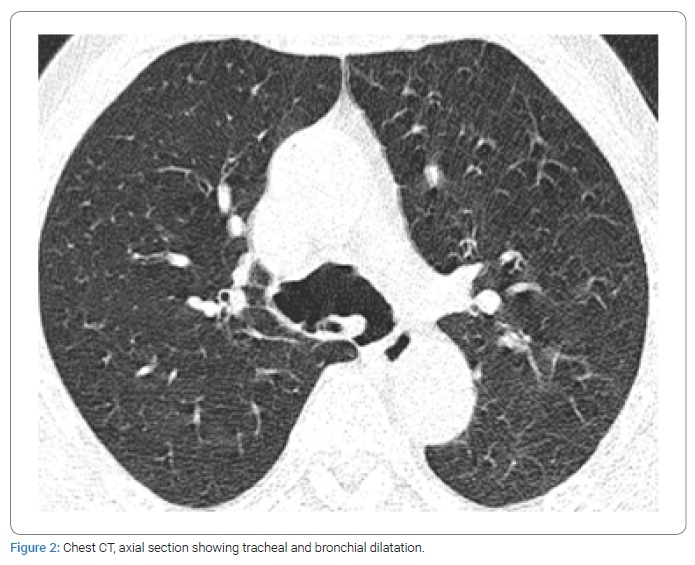
Fibroscopic examination of the bronchi showed a distinction between dilatation of the trachea and the diverticula. The diagnosis of Mounier Kuhn Syndrome or idiopathic tracheobronchomegaly was retained in the absence of etiology explaining the CT scan and bronchoscopy results.
The evolution at 3 months of this disease was marked by the persistence of lower respiratory infections.
Discussion
Tracheobronchomegaly or Mounier Kuhn syndrome is a rare clinical and radiological condition which acquired or congenital origin is still debated. This tracheobronchial dilation may be caused by atrophy of the elastic fibers of the trachea and main bronchi [4]. In the literature, the male gender was the most affected by this disease [5,6]. The clinical presentation is variable, ranging from an asymptomatic manifestation with preserved lung function to severe respiratory failure. For our patient, the clinical manifestation was marked by the recurrence of respiratory infections, bilateral ptosis, clubbing digital and sibilant rale. The diagnosis is confirmed by computed tomography or chest X-ray with a tracheal diameter in coronal and sagittal section greater than 25 mm and 27 mm respectively in men and greater than 21 mm and 23 mm in women and a diameter of the right main bronchus greater than 20 mm and the left main bronchus at 18 mm [7]. For our study, a tracheal diameter in the sagittal section was 39 mm with the presence multiple diverticula. Bronchoscopy confirmed a diagnosis for this disease.
In fact, there are 3 subtypes of mounier khun syndrome. For our case, it was subtype II as there is a distinction between the dilation and diverticula. In type I, there is a slight symmetrical dilation of the trachea and/or the main bronchi while in type III, the diverticular and sacculiform structures extend to the distal bronchi [8]. The respiratory function exploration may be normal or find ventilatory disorders [9]. The spirometry of our patient objectified an obstructive ventilatory disorder. Treatment is usually symptomatic. Chest physiotherapy can be offered to improve mucociliary clearance and antibiotics are administered in case of acute exacerbation of the disease by pulmonary infections [10]. Airway collapse in much selected cases of tracheomalacia can be reduced by placement of a tracheal or tracheobronchial stent, with or without surgical tracheobronchoplasty.
Conclusion
Tracheobronchomegaly is a rare condition whose main characteristic is the dilation of the bronchi and trachea. Most often, it predominates in male subjects. Clinically, there are no pathognomonic signs, its manifestation is variable but can be serious. Chest imaging such as chest computed tomography is essential for diagnosis. Treatment is essentially symptomatic but medical monitoring is essential.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Pulmonary infections; Tracheal and bronchial dilation; Chest CT scan
Cite this article
Razafimpihanina SM, Tiaray Harison M, Razafindrasoa AZ, Andriarimanga DO, Andriamahenina PP, Ramanandafy H, et al. Mounier Kuhn syndrome: first case reported in Madagascar. World J Public Health Epidemiol. 2022;1(1):1–3.
Copyright
© 2022 Razafimpihanina Sonia Marcelle. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).