Abstract
Introduction: Dematiaceous fungi causing corneal infections are rare. Neoscytalidium Dimidiatum a dematiaceous fungus is primarily a plant pathogen rarely causing keratitis.
Case Details: A 67-year-old male patient came to Ophthalmology OPD with history of trauma to right eye followed by redness, itching and other complaints. Gram staining of scrapping from (3 x 3) mm corneal ulcer showed few dark and few hyaline septate fungal hyphae. Culture was identified as Neoscytalidium dimidiatum. Antifungal treatment was started, but patient lost to follow-up.
Conclusion: Neoscytalidium dimidiatum is rare but virulent agent of keratitis. To treat such case early microbiological investigation is necessary.
Abbreviations
OPD: Out Patient Department; ART: Antiretroviral Therapy; USA: United States of America; KOH: Potassium Hydroxide; SDA: Sabouraud’s Dextrose Agar; BA: Blood Agar; CMC: Carboxymethyl Cellulose; DAMA: Discharged Against Medical Advice.
Introduction
In a partial taxonomic revision of the family Botryosphaeriaceae, Crous et al. concluded that Scytalidium is polyphyletic and proposed the genus Neoscytalidium to accommodate Scytalidium dimidiatum as Neoscytalidium dimidiatum [1]. Neoscytalidium dimidiatum a dematiaceous fungi, is primarily plant pathogen which may cause skin and nail infection in human [2,3]. Though moulds are one of common cause of keratitis, Neoscytalidium is a rare culprit [4]. Neoscytalidium dimidiatum was first isolated from keratitis patient (Latin America) by Calvillo [5]. In India, from very few cases of keratitis Neoscytalidium dimidiatum was isolated (Porur, Chennai) [6]. While in world Neoscytalidium dimidiatum was found malfeasant in few countries like Toledo (USA), Riyadh (Saudi Arabia). [7,8] Correlation of fungal keratitis with HIV infection is unclear. HIV causes immune compromised state. According to Mselle 1999 [9], HIV patients are immune compromised so fungal keratitis may be caused in such patients, but studies like Ezisi et al. [10], mention fungal keratitis caused in immune compromised state but didn’t mention direct correlation of HIV with fungal keratitis [9,10]. Majority of study does not mention any direct relation of HIV and fungal keratitis.
Case Report
A 67-year-old male watchman, from low socioeconomic group of Solapur city visited Ophthalmology OPD on October 22, 2019 with main complaints of redness, itching, pain, watery discharge, decreased & blurring of vision of right eye since 2 days. Also history of trauma to same eye with cement and sand 2 days preceding to above complaints. Patient is HIV reactive with ART treatment for more than 5 years. No history of diabetes or hypertension. No history of use of contact lenses or any local application or systemic intake of steroid/antifungal/antimicrobial agent. On local examination of right eye it was found that corneal opacity and ulcer of (3 x 3) mm of size, corneal thinning, 1 mm hypopyon, mild eyelid edema. While vision was of finger counting up to 6 feets (Figure 1).

Bilateral Immature cataract was Incidental finding. Clinician started treatment with provisional diagnosis of “Right eye corneal ulceration with hypopyon”.
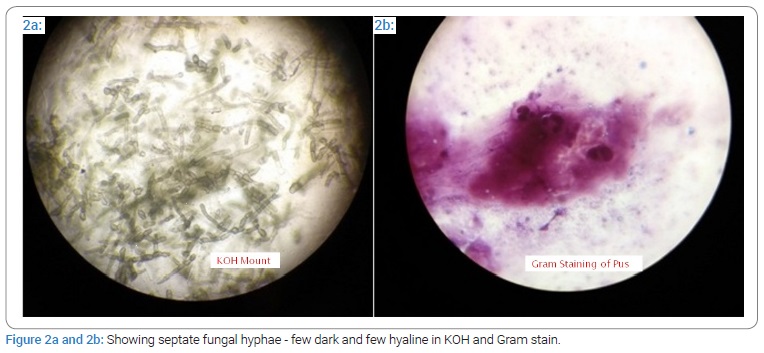
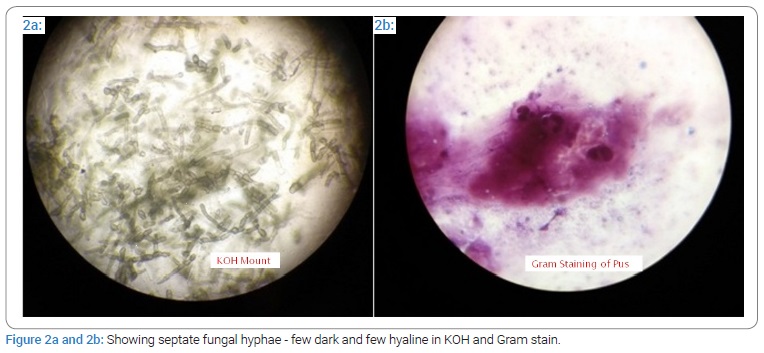
In Microbiology laboratory corneal scrapping was examined. On KOH mount, Septate fungal hyphae few dark and few hyaline was seen. Fungal hyphae were seen on Gram stain of corneal scrapping. While the Gram staining of pus discharge reviled few pus cells and few epithelial cells without any organism (Figure 2a and 2b).
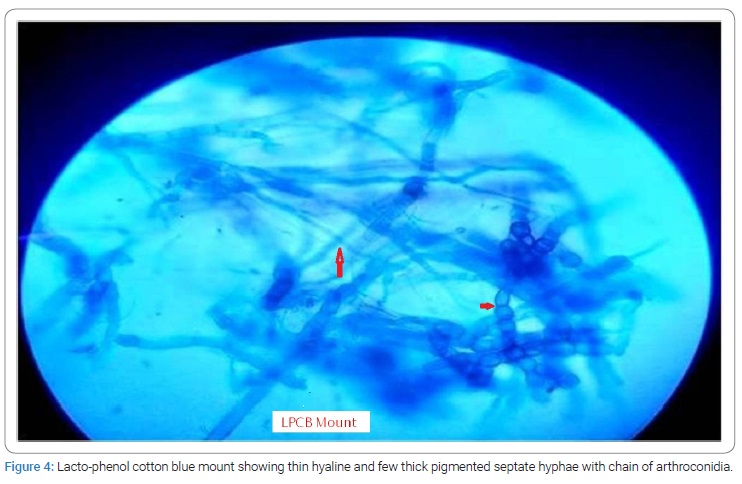
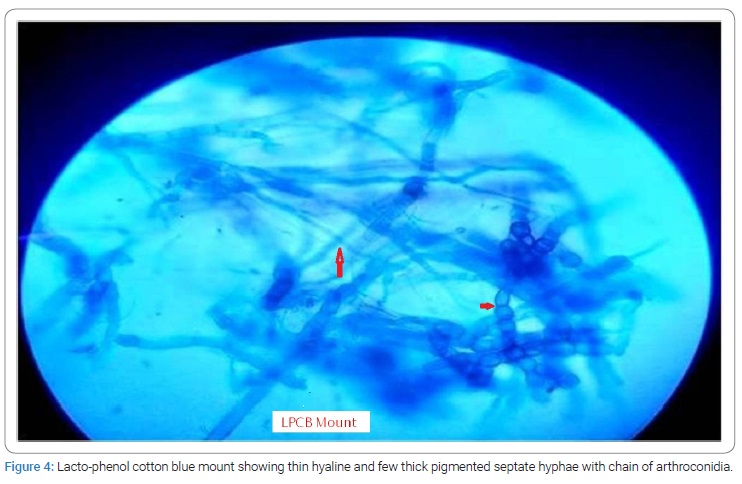
Corneal scrapping was inoculated on Sabouraud’s Dextrose Agar (SDA) and Blood Agar (BA). Third day on SDA there was mycelial growth with grey colour on observe side and darker on reverse (Figure 3a and 3b). On further incubation colonies became more blackish grey. Lacto-phenol cotton blue mount of colony shows thin hyaline septate fungal hyphae & few thick pigmented septate hyphae with chain of arthroconidia (Figure 4).

Patient was put on eye drops of Natamycin, Moxifloxacin, Homatropine hydrobromide (Homide), CMC lubricant. Also Oral Fluconazole 150 mg, Ciprofloxacin 500 mg for 3 days in hospital, analgesic, antacids, and vitamin C was given to patient. Patient was admitted for 2 days and advised to continue hospitalization but patient took Discharged Against Medical Advice (DAMA). During DAMA patient was advised to continue treatment and use dark goggles for protection from light.
When patient visited OPD after 6 days of DAMA for investigation, it was not possible to scrape corneal ulcer edges due to thinning. Hypopyon size was increased from 1 mm to 4 mm, while edema on eyelid was subsided and became normal. Patients condition was worsen in 7 days between follow-up. Further patient was advised for hospital admission for clean corneal scrapping and antifungal therapy, but patient denied. So Patient was advised for local and oral treatment with Natamycin, Voriconazole, MFC, Homide and CMC one hourly, two hourly, two hourly, BD and QID respectively. Voriconazloe was drug of choice. There is no standardized treatment for Neoscytalidium spp infections.
Discussion and Conclusion
In India Aspergillus species (27% to 64%), Fusarium (6% to 32%) and Penicillium (2% to 29%) are main pathogen for keratitis [11]. Neoscytalidium spp is a plant pathogen which is very rarely suspected as agent to keratitis [4]. Neoscytalidium is a thermo tolerant fungus that can cause superficial skin and nail infections that mimic those caused by dermatophytes [12]. Up to 2015 only 5 cases of keratitis by Neoscytalidium are noted worldwide [5]. Only four species of genus Neoscytalidium are identified these are N. dimidiatum, N. oculus, N. orchidacearum, and N. novaehollandiae [13]. Neoscytalidium spp can be cultured in laboratory, but they are morphologically difficult to distinguish from one another [13]. Even though Neoscytalidium is a common plant pathogen, the source of infection in Tendolkar et al. [4], case and present case is non-vegetative (soil and sand) Keratitis is treated empirically without microbiological investigations, but keratitis due to Neoscytalidium dimidiatum very virulent type of infection and also it is difficult to treat and eradicate. So early diagnosis of this causative agent is require to initiate specific treatment as early as possible to obtain rapid and complete recovery.
Anti-fungal treatment is overall lingering and expensive which creates scope to patient to stop treatment and stop follow-up. In this case also patient denied for admission and came for follow-up for just once. Even though patient is on antifungal treatment both oral and local he’s condition worsen. As eye is precious and vital organ, the infection due to Neoscytalidium spp which is invasive in nature and resistant to anti-fungal drugs usually ends in evisceration of eye. Treatment of such infection is possible with extensive IV antifungal treatment which is expensive and for long duration. Also Classical topical treatments against dermatophytes (like griseofulvin, ketoconazole, itraconazole) are often not effective with Neoscytalidium spp, this is possible due to excess of melanin. For successful treatment of such melanin producing mold is obtained with systemic use of azoles (voriconazole and itraconazole) or with amphotericin B. However, in most cases, healing is protracted and combinations of drugs are often necessary [2].
Recommendations
A righteous history and complete eye examination may provide sufficient information to suggest the pathogenesis of the disease and likely microorganisms. We recommend sending corneal scrapping along with complete history which directs microbiologist towards proper and early diagnosis. Unusual Fungal Isolate with correlation of KOH findings should be followed as potential pathogen. A low socio-economy group is risk factor for fungal keratitis. We recommend, to provide all antifungal drugs free of cost completely in government tertiary health care centers.
Acknowledgment
I am very thankful to Dr Sarode Suhas, Professor and Head, Ophthalmology and his team for their support for providing the clinical photograph and details.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Rare fungal keratitis; Management; Neoscytalidium dimidiatum
Cite this article
Dharmshale S, Shinde D, Bali A, Kandle S. A rare fungal isolate Neoscytalidium dimidiatum from keratitis in a people living with HIV. World J Public Health Epidemiol. 2022;1(1):1–4.
Copyright
© 2022 Sujata Dharmshale. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).