Evaluation of Erector Spinae Plane (ESP) Block in He-Patic Surgery: A Case Series
* Giuseppe De Simone;
D’Amico R;
Merciai F;
Marra A;
Nasto RA;
Maresca A;
Troisi RI;
Servillo G;
-
* Giuseppe De Simone: Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy.
-
D’Amico R: Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy.
-
Merciai F: Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy.
-
Marra A: Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy.
-
Nasto RA: Department of Hepato Pancreatico Biliary, Minimally Invasive and Robotic Surgery, Department of Clinical Medicine and Surgery, University of Naples Federico II, Naples, Italy.
-
Maresca A: Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy.
-
Troisi RI: Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy.
-
Servillo G: Department of Neurosciences, Reproductive and Odontostomatological Sciences, University of Naples Federico II, Naples, Italy.
-
Jul 19, 2022 |
-
Volume: 1 |
-
Issue: 1 |
-
Views: 1482 |
-
Downloads: 1003 |
Abstract
A Pain management is a pivotal aspect for Enhanced Recovery After Surgery (ERAS). Intrathecal morphine (ITM) is the current gold standard for postoperative pain management following hepatic surgery. Erector Spinae Plane (ESP) block is a novel regional anesthesia technique used as part of multimodal analgesia for several surgical procedures; nevertheless, data on its efficacy and safety in hepatic surgery are limited. We report our experience with ESP-block for pain management in 3 patients who underwent liver resection through 3 different approaches: (1) laparotomic, (2) laparoscopic, and (3) robot assisted. ESP block consisted of a bilateral injection of a 20 mL 0.5% ropivacaine solution at T7 before induction of general anesthesia. Postoperative pain was evaluated using Numeric Rate Scale (NRS) and Visual Analog Scale (VAS) scores. ESP-block demonstrated an effective analgesia especially in patient subjected to mini-invasive approaches (laparoscopy and robot–assisted surgery) and less opioid requirement after surgery and during hospital stay.
Abbreviations
TAP: Transversus Abdominal Plan; IV: Intra-Venous; NSAIDs: Non Steroidal Anti-Inflammatory Drugs; ESP: Erector Spinae Plan; TEA: Thoracic Epidural Analgesia; ITM: Intrathecal Morphine; PONV: Post Operative Nause and Vomiting; LOS: Length of Stay; NRS: Numerical Rating Score; VAS: Visual Analog Scale; SC: Subcutaneous; METS: Measurement of Exercise Tolerance before Surgery; ASA: American Society of Anesthesiologist; POD: Post Operative Day; PCA: Patient Controlled Analgesia; ERAS: Enhanced Recovery After Surgery; ICU: Intensive Care Unit; MAC: Minimum Alveolar Concentration; OR: Operating Room; SBP: Systolic Blood Pressure; DBP: Diastolic Blood Pressure; HR: Heart Rate
Introduction
Postoperative pain management is a key component of Enhanced Recovery After Surgery (ERAS) protocol [1]. Multimodal analgesia as part of an ERAS protocol facilitates early mobility, early return of bowel function, adequate ventilator mechanics, and preventing thromboembolic events and pneumonia and decreases postoperative morbidity [2]. Patients undergoing hepatic surgery are at considerable risk of perioperative complications [3], including thromboembolic events, pulmonary [4], nausea and adverse digestive events, liver and renal failure [5].
While Thoracic Epidural Analgesia (TEA) and Intra-Venous (IV) opioid Patient-Controlled Analgesia (PCA) are the gold standard for upper abdominal surgery [6], hepatic surgery poses further challenges for pain management due to the risk of coagulopathies, biliary tract obstruction, intraoperative blood loss and reduced metabolic liver function.
The standard analgesic regime at our institution, for major hepatic surgery, includes pre-induction Intrathecal Morphine (ITM) (dose 8 μg/kg to 10 μg/kg, ideal body weight), subcostal Transversus Abdominal Plan (TAP) blocks [7], and additional administration of paracetamol and Non-Steroidal Anti-inflammatory Drugs (NSAIDs) when appropriate.
Erector Spinae Plane (ESP) block, described by Forero et al. in 2016 [8], is a simple and safe ultrasound guided interfacial plane block due to the fact that the sono-anatomy is detectable and there are no structures at risk of needle injury, providing both somatic and visceral analgesia.
To date, many papers have been published describing the use of the ESP-block in different medical scenarios but only a few studies evaluated the role of ESP-block in hepatic surgery. The aim of this study was to describe our experience with ESP-block for pain control in three patients undergoing liver research surgery using open and minimally invasive approach (i.e. laparoscopy and robot-assisted).
Methods
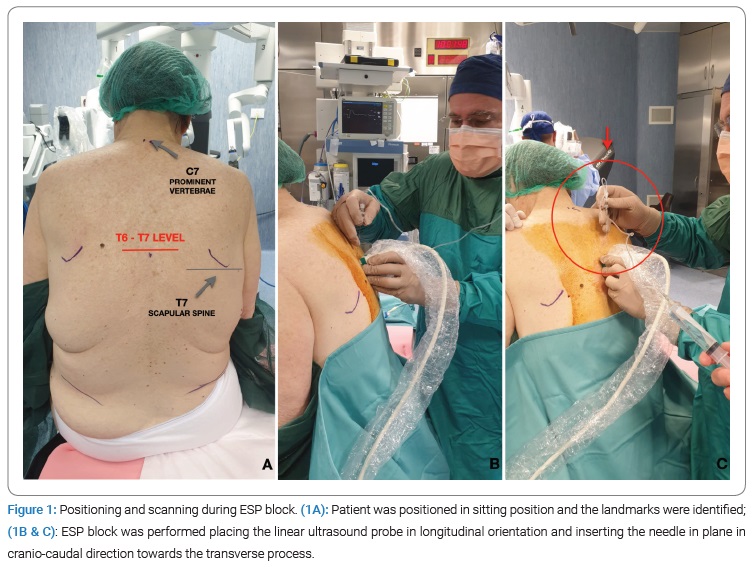
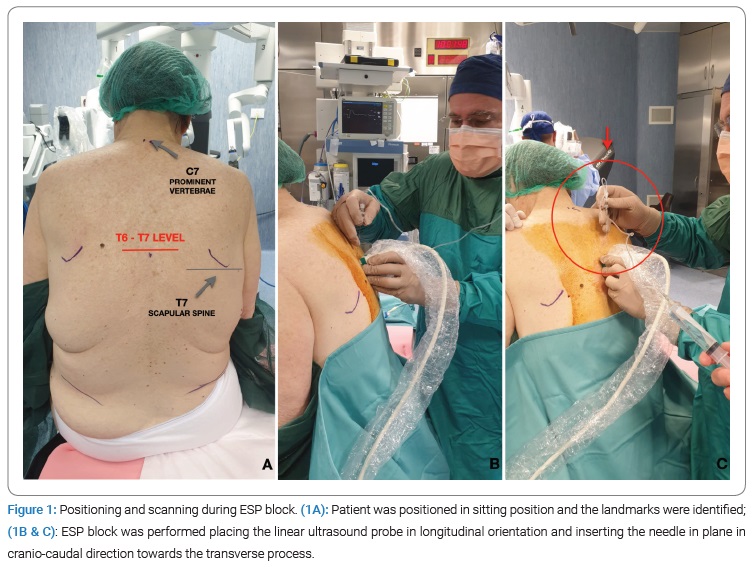
We retrospectively reviewed clinical charts of a consecutive series of 3 patients who underwent liver resection surgery at our institution (written consent has been obtained from the patients for publication of this case report). All patients were scheduled for elective liver resection with different surgical approach: (1) laparotomic, (2) laparoscopic, and (3) robot assisted. Signed informed consent was obtained from all patients. ESP-block was performed before induction of general anesthesia. ESP-block was performed, in a sitting position, under ultrasound guidance using a linear (6 to10) MHz ultra-sound probe. We performed a preliminary scan to define and mark spinous processes at T6-T7 level (Figure 1A). The linear ultrasound probe was placed in a longitudinal parasagittal orientation 3 cm lateral to the T7 spinous process (Figure 1B). A100 mm 22 G needle (Vygon) was inserted under ultrasound guidance in plane in cranio-to-caudal direction, underneath the erector spine muscle, towards the transverse process (Figure 1C), injecting a total of 20 ml of 0.5% ropivacaine. The technique was repeated on the other side.
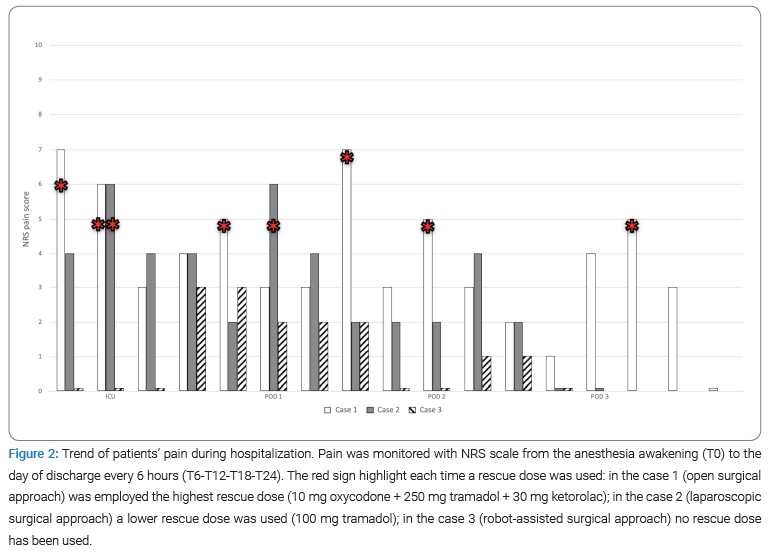
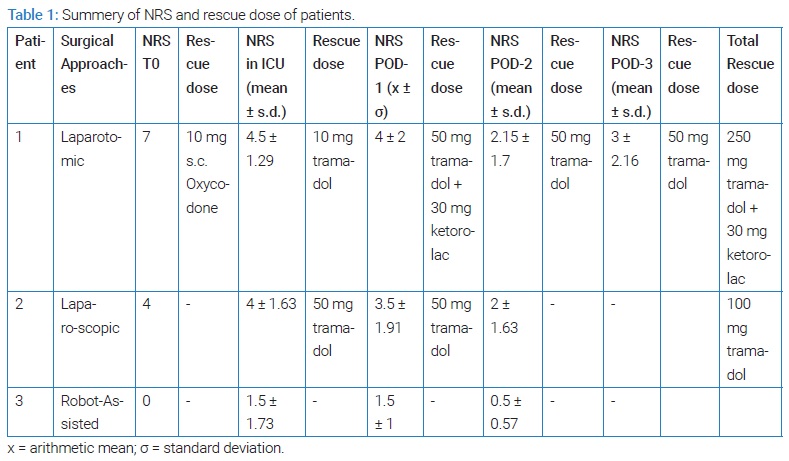
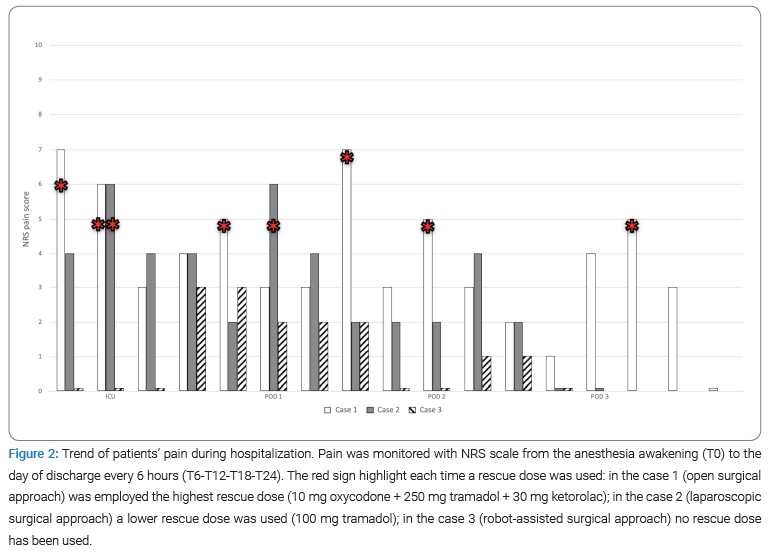
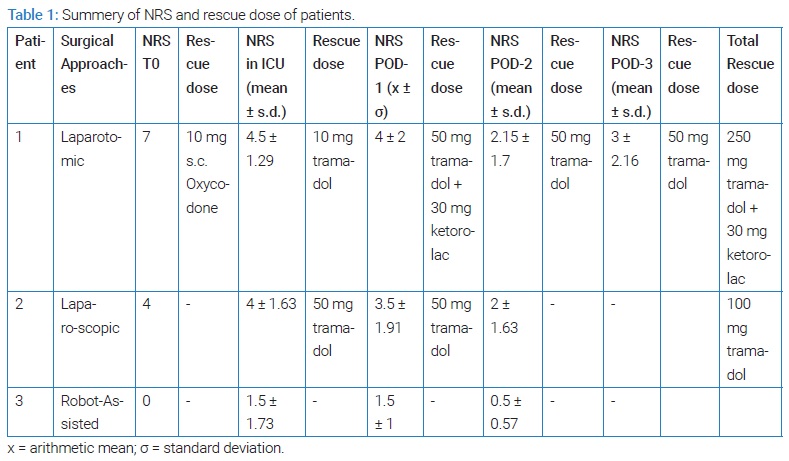
General anesthesia was induced with fentanyl (1 μg/kg to 2 μg/kg), propofol (1.5 mg/kg to 2 mg/kg), cisatracurium (0.2 mg/kg) and was maintained with desflurane (MAC 0,8) in oxygen and air in equal concentration and remifentanyl 0.05 - 0.25 μg/kg/min. Thirty minutes before the end of surgery, the patient received 1 g paracetamol. The patients were extubated at a TOF ratio of 100%. At the end of surgery, pain was evaluated using Numerical Rating Score (NRS) and Visual Analog Scale (VAS) score. If pain score was > 6/10 at the NRS scale, 10 mg subcutaneous (s.c.) oxycodone were administered. Patients were transferred to the Intensive Care Unit (ICU) for further surveillance for 24 hours. The patients’ pain was monitored with NRS and VAS scales, from the anesthesia awakening (T0) to the day of discharge every 6 hours (T6-T12-T18-T24), for all time of hospitalization (Figure 2). All patients were followed using a standardized postoperative analgesia protocol, which included 1 g paracetamol every 8 hours for the 48 hours after surgery. In case of NRS or VAS score > 4/10, a rescue dose of 50 mg tramadol was given, maximum twice daily. In case of NRS or VAS score > 6/10, a rescue dose of 50 mg tramadol + 30 mg ketorolac was given, maximum three times per day (Table 1).
Case Presentation
Case 1
An adult woman, BMI of 32 kg/m2, was scheduled for laparotomic caudate lobe resection for suspected HCC. Hepatic status was Child Pugh Score A6, MELD Score 8 and platelet count before surgery was 170000/uL. American Society of Anesthesiologist (ASA) physical status was II. The surgical approach consisted of a right subcostal incision with a median split to the xiphoid process and positioning of Thompson Retractors. Time of surgery was 430 minutes. Intraoperative remifentanyl dose range was 0.04 μg/kg/min to 0.2 μg/kg/min. The patient remained hemodynamically stable during the whole surgical procedure and did not require any vasopressor drug.
The mean values of Systolic (SPB) and Diastolic (DBP) blood pressures were 110 mmHg and 64 mmHg, respectively. Average Heart Rate (HR) was 66 bpm and SpO2 99%. The patient upon awakening from anesthesia (Aldrete Score 10/10) reported pain 7/10 NRS (T0), and 10 mg of oxycodone s.c were given. She did not present any episodes of PONV. In ICU, NRS pain score was 6/10 at T6, and 50 mg of tramadol was given. At T12, NRS was 3/10 and at T18 was 4/10. At T24 NRS and VAS was 5/10 and 50 mg tramadol was administered. At T18 of Post Operative Day (POD)-1, NRS and VAS were 7/10 and 50 mg tramadol plus 30 mg of ketorolac was administered. At T24, NRS was 3/10. At T6 of POD-2, NRS and VAS were 5/10 and a rescue dose of 50 mg of tramadol was given. At T12 of POD-2 NRS and VAS was 3/10. During the last time (T18-T24) of the POD-2, reported pain was not significant. At T12 of POD-3, NRS and VAS were 5/10 and we used 50 mg of tramadol (Figure 2). The patient was mobilized on the POD-1. Bowel function recovered on POD-2. Patient was discharged on POD-4.
Case 2
An adult woman, BMI 22.2 kg/m2, scheduled for laparoscopic left lateral liver resection and nodules ablation of fifth and seventh segments for suspected HCC lesion. The hepatic status was Child-Pugh Score A5, MELD score 25, platelets count 271000/uL. ASA risk score was III. The surgical procedure was performed through a standard laparoscopic approach with 4 ports. Intraoperative mean values of SBP and DBP were 117 mmHg and 48 mmHg, respectively. Average HR was 49 bpm and SpO2 99%. Intraoperative remifentanyl dose range was 0.02 μg/kg/min to 0.12 μg/kg/min. Surgical procedure lasted 360 minutes. NRS at extubation (T0) was 4/10. At T6, patient reported NRS pain score of 6/10, and a tramadol rescue dose was administered. At T12 and T18, NRS was 4/10. At T6 of POD-1, NRS and VAS were 6/10 and 50 mg of tramadol was given. During the last time of POD-1, the mean values of NRS and VAS were less than 3/10. Also on POD-2, the strongest pain was 4/10 on NRS and VAS at T12 (Figure 2). The patient was mobilized on POD-1. During POD-2 bowel function recovered. In the morning of POD-4 patient was discharged.
Case 3
A middle-aged man, BMI of 25.7 kg/m2, with suspected HCC nodule in the V liver segment was scheduled for robotic-assisted segmentectomy e cholecystectomy. Medical history included portal hypertension with gastric varices IGV1. The hepatic status was Child-Pugh Score B8, MELD score 14, platelets count 46000/uL. Surgery duration was 315 minutes. The mean values of SBP and DBP were 112 mmHg and 54 mmHg, respectively. HR was 74 bpm and SpO2 100%. Intraoperative remifentanyl dose range was 0.02μg/kg/min to 0.1μg/kg/min. Norepinephrine at a mean dosage of 0.1 μg/kg/min was used during surgery, and it was weaned 30 minutes before the end of the procedure. At T0 patient reported NRS pain score 0/10 (T0). The pain was almost absent, except for T18 and T24, that was 3/10 on NRS and 2/10 on VAS. In POD-1 pain was under control in fact patient referred at T6, T12 and T18, 2/10 on NRS and 1/10 on VAS, and at T24 0/10 on NRS and VAS (Figure 2). In this case was not necessary to use rescue doses at the weakening and during the hospitalization. Patient was mobilized on the POD-1 and, bowel function resumed on POD-2. Patient was discharged on POD-3.
Discussion
In our experience ESP-block demonstrate an effective analgesia especially in patient subjected to mini-invasive approaches (laparoscopy and robot–assisted surgery) and a significant decrease of opioids consumption in the peri-operative period. This resulted in an early mobilization of our patients and quicker recovery of the bowel function after surgery.
Peri-operative pain management in hepatic surgery is an area of active investigation and still controversial. Literature shows how the use of ESP-block in hepatic surgery is still sparse. TEA and ICT are commonly used [9], but newer techniques have been advocated. A study performed with Contrast-Enhanced MRI observing the real diffusion of the local anesthetic, shows drug spreading along the length of the thoracolumbar spine in the interfascial plane between the transverse processes and the erector spinae muscles, acting on the dorsal and ventral rami of spinal nerves. In a minimal part of patients, the blockage spreads also to the epidural plane and the great advantage is that it provides both somatic and visceral analgesia [10]. To our knowledge only 4 works described the effect of ESP-block in hepatic surgery: Shrijit Nair et al. [11] and Upendra et al. [12] performed ESP-block at T7 and placed bilateral ESP catheters for analgesia, infusing local anesthetic for more days. Gulcin Hacibeyoglua et al. [13] performed bilateral block at T8 after induction of anesthesia, while Kang et al. [14] compared the use of bilateral ESP-block with ITM. Unlike us, all these authors do not always report the NRS value used to administer the rescue dose and the average opioids consumption in PODs is higher. Moreover, LoS are significantly longer. According to ERAS protocol ITM is the preferred technique, epidural injections should be used with caution in patients at high risk of coagulopathies and possible prolonged time of prothrombin after hepatectomy [15,16]. ITM provides a good pain control but has significant adverse effects such as frequent PONV, itching and the potential for delayed respiratory depression [17]. Adhikary et al. [18] demonstrated that the use of ESP-block in polytrauma patients is preferable to TEA because of the lower risk of hypotension, urinary retention and pneumothorax.
In our center, we use ITM to control postoperative pain in major abdominal surgery; 200 μg morphine + 7.5 mg of 0.75% ropivacaine are injected, with a satisfactory pain control for 18 hours to 20 hours. However, this technique can be associated with sensory disorders and late alvus normalization with a longer LoS. The aim of introduction ESP-block in our clinical practice was to overcome these limitations. Patients showed an early mobilization and they were all discharged with no pain, open bowels, and oral feeding. The average LoS in our case series was 3.5 days after surgery, while in a prospective cohort study, of 73 patients undergoing hepatic resection the median LoS was 13 days in thoracic epidural analgesia and 11 day in intrathecal morphine [19]. Thanks to the association of constant respiratory physiotherapy and appropriate hydration, combined with pain control, we did not observe any pulmonary complications (e.g. pulmonary embolism, pleural effusion and basal atelectasis) and the patients did not need more than 24 hours in ICU. In our experience ESP-block could be considered valid strategies for hepatic surgery in both open and minimally invasive approaches. The introduction of ESP block in our analgesia protocol yielded results comparable to intrathecal morphine, reducing the risk and failure rate associated with technique. Future work is needed to define better the safety and the efficacy of ESP block in hepatic surgery.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Jacquenod P, Wallon G, Gazon M, Darnis B, Pradat P, Virlogeux V, et al. Incidence and risk factors of coagulation profile derangement after liver surgery: implications for the use of epidural analgesia-a retrospective cohort study. Anesth Analg. 2018;126(4):1142–1147.
- Kneuertz PJ, Pitt HA, Bilimoria KY, Smiley JP, Cohen ME, Ko CY, et al. Risk of morbidity and mortality following hepato-pancreato-biliary surgery. J Gastrointest Surg. 2012;16(9):1727–1735.
- Sydow FW. The influence of anesthesia and postoperative analgesic management of lung function. Acta Chir Scand Suppl. 1989;550:159–165.
- Dokmak S, Ftériche FS, Borscheid R, Cauchy F, Farges O, Belghiti J. 2012 Liver resections in the 21st century: we are far from zero mortality. HPB (Oxford). 2013;15(11):908–915.
- Verhoef C, Singla N, Moneta G, Muir W, Rijken A, Lockstadt H, et al. Fibrocaps for surgical hemostasis: two randomized, controlled phase II trials. J Surg Res. 2015;194(2):679–687.
- Salicath JH, Yeoh EC, Bennett MH. Epidural analgesia versus patient-controlled intravenous analgesia for pain following intra-abdominal surgery in adults. Cochrane Database Syst Rev. 2018;8(8):CD010434.
- Milone M, Di Minno MN, Musella M, Maietta P, Iacovazzo C, Milone F. Ultrasound-guided transversus abdominis plane block for retroperitoneal varicocele repair. Could it be an anesthesia method?. Updates Surg. 2013;65(3):225–230.
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–627.
- De Pietri L, Siniscalchi A, Reggiani A, Masetti M, Begliomini B, Gazzi M, et al. The use of intrathecal morphine for postoperative pain relief after liver resection: A comparison with epidural analgesia. Anesth Analg. 2006;102(4):1157–1163.
- Schwartzmann A, Peng P, Maciel MA, Alcarraz P, Gonzalez X, Forero M. A magnetic resonance imaging study of local anesthetic spread in patients receiving an erector spinae plane block. Can J Anaesth 2020;67(8):942–948.
- Nair S, Mc Guinness S, Masood F, Boylan JF, Conlon NP. Erector spinae plane blocks in major hepatopancreaticobiliary surgery: a case series. A A Pract. 2019;13(9):332–334.
- Maddineni U, Maarouf R, Johnson C, Fernandez L, Kazior MR. Safe and effective use of bilateral erector spinae block in patient suffering from post-operative coagulopathy following hepatectomy. Am J Case Rep. 2020;21:e921123.
- Hacibeyoglua G, Topala A, Aricana S, Kilicaslana A, Tekinb A, Uzuna ST. USG guided bilateral erector spinae plane block is an effective and safe postoperative analgesia method for living donor liver transplantation. J Clin Anesth. 2018;49:36–37.
- Kang RA, Chin KJ, Gwak MS, Kim GS, Choi SJ, Kim JM, et al. Bilateral single-injection erector spinae plane block versus intrathecal morphine for postoperative analgesia in living donor laparoscopic hepatectomy: a randomized non-inferiority trial. Reg Anesth Pain Med. 2019;rapm–2019–100902.
- Roy JD, Massicotte L, Sassine MP, Seal RF, Roy A. A comparison of intrathecal morphine/fentanyl and patient-controlled analgesia with patient-controlled analgesia alone for analgesia after liver resection. Anesth Analg. 2006;103(4):990–994.
- Sakowska M, Docherty E, Linscott D, Connor S. A change in practice from epidural to intrathecal morphine analgesia for hepato-pancreato-biliary surgery. World J Surg. 2009;33(9):1802–1808.
- Wheeler M, Oderda GM, Ashburn MA, Lipman AG. Adverse events associated with postoperative opioid analgesia: a systematic review. J Pain. 2002;3(3):159–180.
- Adhikary SD, Liu WM, Fuller E, Cruz-Eng H, Chin KJ. The effect of erector spinae plane block on respiratory and analgesic outcomes in multiple rib fractures: a retrospective cohort study. Anaesthesia 2019; 74(5):585–593.
- Kasivisvanathan R, Abbassi-Ghadi N, Prout J, Clevenger B, Fusai GK, Mallett SV. A prospective cohort study of intrathecal versus epidural analgesia for patients undergoing hepatic resection. HPB (Oxford). 2014;16(8):768–775.
Keywords
TESP block; Opioids sparing; Pain management
Cite this article
Simone GD, D’Amico R, Merciai F, Marra A, Nasto RA, Maresca A, et al. Evaluation of erector spinae plane (ESP) block in he-patic surgery: a case series. Ann Neur Res Stud. 2022;1(1):1–5.
Copyright
© 2022 Giuseppe De Simone. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).