Abstract
Background and Objectives: Neurological manifestations of acute COVID-19 infection have been reported, here we evaluate a case series of newly diagnosed patients with multiple sclerosis after acute COVID-19 infection.
Methods: Patients were included based on the present criteria: Patients were diagnosed with Relapsing-Remitting Multiple Sclerosis (RRMS) based on 2017 McDonald criteria up to 6 weeks after having an acute COVID-19 infection.
Results: A total of 10 patients were included. 50% were male, mean age of 28. Average time to neurological presentation was between 2 weeks to 6 weeks after active COVID-19 infection. Partial transverse myelitis was evident in 40% of the cases. All patients presented with enhancing lesions in brain MRI, 6 patients also had spinal cord involvement. Presence of CSF oligoclonal bands was found in all cases. The majority of patients (80%) were unvaccinated for COVID-19.
Conclusion: COVID-19 infection has been linked to several neurological conditions. This study documents that in susceptible individuals it can work as a trigger for developing relapsing-remitting MS.
Introduction
Neurological manifestations of COVID-19 have been now well-documented. Active COVID-19 infection has been recognized as a trigger for an MS exacerbation [1]. Recent study documented that more than one-third of patients with COVID-19 developed neurological complications during the acute phase, and more than one-third developed neuropsychiatric complications 6 months after infection [2]. Here, we are evaluating a group of patients who were diagnosed with Relapsing Remitting MS after an acute COVID-19 infection.
Method
Patients who fulfilled the 2017 McDonald criteria for RRMS presenting between weeks 2 to 6 after COVID-19 infection were included. Patients with previous MS diagnosis or report of neurologic symptoms suggestive of MS prior to COVID-19 infection were excluded. Demographic data as well as clinical and radiographic information was obtained. MS mimickers were ruled out. Patients verbally consented to participate in this case report.
Results
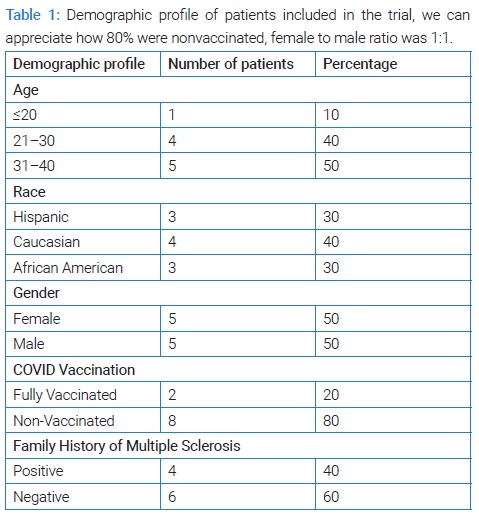
Ten patients were included, all fulfilled 2017 McDonald criteria for Relapsing Remitting MS and presented between weeks 2 to 6 after an active COVID-19 infection. Ninety percent of patients developed their first neurologic symptom consistent with an MS relapse after their first COVID infection; 80% of patients were not vaccinated for COVID-19. The sex ratio was 1:1 with a mean age of 28. The rest of demographic information is presented in (Table 1). Most (90%) of patients had mild COVID-19 symptoms consisting of loss of taste and mild flu-like symptoms, only one patient had nausea, vomiting and fever with no loss of smell or taste. None of the patients were hospitalized for COVID-19 symptoms.
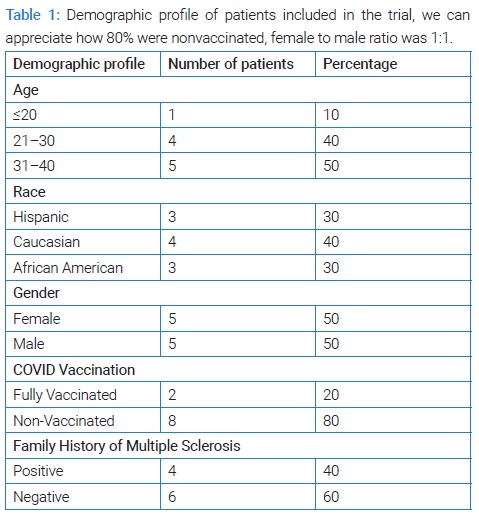
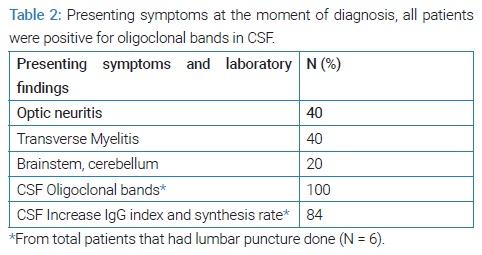
Clinical manifestation of multiple sclerosis developed during the patient’s recovery from COVID-19 related symptoms in all cases between weeks 2 and 6. Neurological presentation was variable (Table 2) with 40% of the patients presenting with spinal cord involvement (partial transverse myelitis), 40% with optic neuritis, and 2 patients with brainstem and/or cerebellar involvement.
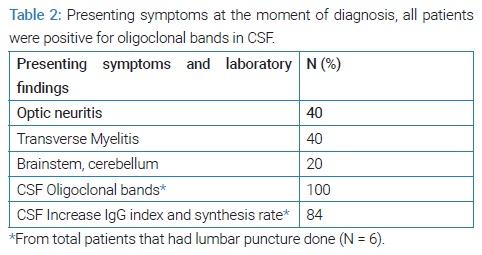
Epstein-Barr virus IgG was tested in 6 patients, and positive in 100% of tested cases. CSF analysis was performed in six cases and was positive for oligoclonal in 100% of the tested cases. 80% of patients had good response to steroids (1 g of Solu-Medrol IV for 5 days). 2 male patients of African descent had a more aggressive course and only partial improvement. Nine out of the ten patients were started on disease modifying therapy, 7 on B-cell therapy (Ofatumumab), one on glatiramer acetate and one on natalizumab.
Discussion
Infectious environmental trigger of MS disease exacerbation has been recognized [3]. There seems to be a strong association with previous Epstein-Barr virus infection and the development of MS [4]. COVID-19 infection has been suggested to induce autoimmune disease. There are multiple reports of autoantibodies in particular anti-cardiolipin, anti-β2-glycoprotein I, and antinuclear antibodies in patients with active COVID-19 infection [5]. Coronavirus family has also shown to have neurotropic properties, triggering secondary demyelination likely by activated T lymphocytes, activated microglia and other inflammatory mediators [6]. It has also been postulated that the virus can spread locally through the cribriform plate of the ethmoid bone where it is believed to cause the olfactory symptoms [6].
There are a few case reports in the literature of a newly diagnosed MS with concurrent COVID-19 infection [6]. It has been recently reported that immune cells infected by COVID-19 can trigger massive inflammatory response by monocytes and macrophages, as well as convincing evidence that the virus can infect and replicate in immune cells and activate inflammasomes which are large molecules that trigger a cascade of inflammatory responses that end in cell death [7]. Close analysis of macrophages in the lungs of patients who had COVID-19 and died show that about one quarter of the cells had activated Inflammasomes. Recent study conducted at Yale University found that the virus could infect and replicate in macrophages in human lungs and as well in a mouse model of the human immune system [7].
The association between COVID-19 infection and the diagnosis of multiple sclerosis remains unclear but nevertheless it may be that the active COVID-19 infection unmasks or triggers the immune system contributing to the development of multiple sclerosis.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
COVID 19 infection; Neuropsychiatric complications of COVID 19; Acute COVID-19; Macrophages
Cite this article
Avila M, Tan Y, Hernandez R, Lara A, Sandoval M. Multiple sclerosis after acute COVID 19 infection. Ann Neur Res Stud. 2022;1(1):1–3.
Copyright
© 2022 Mirla Avila. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).