Risk Factors Associated With the Appearance of the Severe Form of COVID-19 in the Pulmonology Departments of Antananarivo, Madagascar
* Razafimpihanina Sonia Marcelle;
Ramandray F;
Rasoafaranirina MO;
Rakotondrabe DI;
Razafindrasoa AZ;
Andriarimanga DO;
Rakoto AW;
Andriamahenina PP;
Rafitoharson LE;
Rebasy L;
Nandimbiniaina AM;
Ravahatra K;
Rakotomizao JR;
Tiaray Harison M;
Rakotoson JL;
Raharimanana RN;
-
* Razafimpihanina Sonia Marcelle: Department of Medicine, University Hospital Center of Fenoarivo, Antananarivo, Madagascar.
-
Ramandray F: Centre de Recherche pour le Développement, Université Catholique de Madagascar, Madagascar.
-
Rasoafaranirina MO: Department of Medicine, University Hospital Center of Tambohobe, Fianarantsoa, Madagascar.
-
Rakotondrabe DI: Department of Medicine, University Hospital Center of PZAGA, Majunga, Madagascar.
-
Razafindrasoa AZ: Department of Medicine, University Hospital Center of Fenoarivo, Antananarivo, Madagascar.
-
Andriarimanga DO: Department of Medicine, University Hospital Center of Fenoarivo, Antananarivo, Madagascar.
-
Rakoto AW: Department of Medicine, University Hospital Center of Joseph Raseta Befelatanana, Antananarivo, Madagascar.
-
Andriamahenina PP: Department of Medicine, University Hospital Center of Fenoarivo, Antananarivo, Madagascar.
-
Rafitoharson LE: Department of Medicine, University Hospital Center of Tambohobe, Fianarantsoa, Madagascar.
-
Rebasy L: Department of Medicine, University Hospital Center of Fenoarivo, Antananarivo, Madagascar.
-
Nandimbiniaina AM: Department of Medicine, University Hospital Center of Joseph Raseta Befelatanana, Antananarivo, Madagascar.
-
Ravahatra K: Department of Medicine, University Hospital Center of Fenoarivo, Antananarivo, Madagascar.
-
Rakotomizao JR: Department of Medicine, University Hospital Center of Joseph Raseta Befelatanana, Antananarivo, Madagascar.
-
Tiaray Harison M: Department of Medicine, University Hospital Center of Joseph Raseta Befelatanana, Antananarivo, Madagascar.
-
Rakotoson JL: Department of Medicine, University Hospital Center of Joseph Raseta Befelatanana, Antananarivo, Madagascar.
-
Raharimanana RN: Department of Medicine, University Hospital Center of Fenoarivo, Antananarivo, Madagascar.
-
Oct 17, 2022 |
-
Volume: 1 |
-
Issue: 2 |
-
Views: 860 |
-
Downloads: 903 |
Abstract
Introduction: Pneumonia induced by the new virus called "severe acute respiratory syndrome coronavirus 2" or SARS-CoV-2 has killed more than three million people worldwide. This disease is a public health problem especially in a country like Madagascar. The aim of this study is to describe the epidemioclinical profile of patients with COVID-19 and to identify the factors associated with severe forms.
Methods: This is a retrospective, descriptive and analytical cohorte study based on the complete medical records of hospitalized patients who tested positive for COVID-19 at the JRB and Fenoarivo CHUs of seven months, period from March to September 2020.
Results: We registered one hundred and eighty patients infected with SARS-Cov-2 whose average age was 52 years. The male gender was predominant in this study. Only 12.3% of patients were smokers. The clinical manifestation was dominated by the triad cough, dyspnea and asthenia. Advanced age (OR: 2.23; CI: [1.03–4.81]; p-value: 0.04), male gender (OR: 2.44; CI: [1.25–4.75]; p-value: 0.008), and the number of co morbidities greater than 1 (OR: 2.74; CI: [1.13–6, 6]; p-value: 0.01) were significantly associated with the onset of a severe form of COVID-19. Hypertension and diabetes were not among the risk factors. Smoking had a significant odds ratio (OR: 0.29; CI: [0.09–0.9]; p-value: 0.04), but was associated with the non-severe form.
Conclusion: The severe form is particularly found in male patients and those with advanced age or multiple co-morbidities.
Introduction
Pneumonia induced by the new virus called "severe acute respiratory syndrome coronavirus 2" or SARS-CoV-2 has killed more than three million people worldwide. This infectious disease has been named COVID-19 by the World Health Organization (WHO); “CO” for Corona, “VI” for Virus, “D” for Disease and “19” the year it appeared. This virus was first found in Wuhan, Hubei Province, China, in December 2019, and has spread around the world, becoming a pandemic [1–3].
During this pandemic, medical facilities in many countries were overwhelmed with the treatment of severe forms [4]. Compared with severe acute respiratory syndrome coronavırus-1 (SARS-CoV-1) and Middle East Respiratory Syndrome (MERS), COVID-19 has lower mortality [5–7]. The clinical presentation of COVID-19 is polymorphic, ranging from asymptomatic manifestation to severe forms. The release of cytokines and markers of inflammation due to the invasion of the SARS-CoV-2 virus in epithelial alveolar cells type II can cause severe symptoms. This influx of cytokines recruits neutrophils and T cells, which in turn lead to lung damage and significant inflammation, resulting in acute respiratory distress syndrome [8].
In the literature, studies carried out in some countries have found that patients with older age and underlying comorbidities, including diabetes, hypertension and coronary heart disease, are at risk of developing a severe form of COVID-19 and cause death [9–11]. To our knowledge, no study explaining the severe form of COVID-19 for confirmed patients has been carried out in Madagascar whereas, according to Ouédraogo et al. [12], these factors may vary from region to region. Thus, the objective of this article is to identify the risk factors for developing a severe form of COVID-19 in patients received in the Pneumology Departments of the University Hospital Center (CHU) of Antananarivo, Madagascar.
Methods
Study Sample
This research study is a retrospective cohort during the period between March and September 2020, carried out at the USFR (Unit of Care, Training and Research) of Pneumology of the CHU Joseph Raseta of Befelatanana and the CHU of Fenoarivo. Medical records of patients confirmed to have SARS CoV-2 infection were reviewed.
Data was collected from patients who tested positive for SARS CoV-2 from a Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) test on nasopharyngeal and throat swab samples. The data extracted included only demographic data (age, sex and occupation) and clinical data (respiratory and non-respiratory symptoms and vital signs at admission including Pulse Oxygen Saturation SpO2). Laboratory and imaging data were not part of the parameters to be studied because of the lack of data. Pulsed oxygen saturation (SpO2) in ambient air without oxygen therapy was systematically measured by a pulse oximeter as soon as the patient was hospitalized. Referring to the study by David et al. [13], the diagnosis of severe forms was made on the basis of clinical severity criteria: SpO2 less than < 93% in ambient air and respiratory rate greater than 30 cycles/min.
During the preparation of the study, the anonymity of the patients, the individual protection measure and the authorization of the Directors of the Establishment as well as that of the Heads of the Pneumology Department of the 2 CHUs concerned before accessing the data concerning the patient have been complied with.
Statistical Analysis
In this study, the nature of the research is quantitative empiricism with causal inference. Based on the previous works, carried out by Ouedraogo et al. [12], Wang et al. [14], Griffith et al. [15], on different countries, we selected 5 variables such as age ( > 45), smoking, gender (male), hypertension and diabetes (or the number of comorbidities, ≥ 1 and ≥ 2). They have been transformed into a dummy variable and then included in a logistic regression model. The latter is used to estimate the value of the Odds-Ratio (OR) and its 95% Confidence Interval (CI). Also, the descriptive analyses of the variables were also considered, by calculating the mean, the standard deviation and the percentage.
Four equations are estimated in the present study and represented as the estimates (1), (2), (3), and (4).In the estimate (1), we included the different types of comorbidity and demographic characteristics while the estimate (2) includes the number of comorbidities for each patient, excluding demographic characteristics. For these two estimates, the dependent variable is the clinical form of COVID-19 based on SpO2 criteria and respiratory rate. Later, we decided to study the clinical form by including only the criterion of pulsed O2 saturation, which is considered in the estimates (3) and (4). The software used for the statistical analyzes is STATA (version 15.0).
Results
Population Demographics and Clinical Characteristics
Over the course of seven months, a total of 404 patients suspected of covid19 were hospitalized at the USFR Pneumology of the CHU JRB and the CHU of Fenoarivo, of which 217 tested negative and 187 positive. Patients with a positive COVID-19 test and with complete data were included in the study. The total number of patients is thus 180. Among these patients, 122 (67.67%) presented severe forms of covid19 and 58 (32.22%) non-severe forms. (Table 1) summarizes the demographic and clinical data of patients who tested positive for coronavirus.
In this study, the mean age and standard deviation of all patients were 52 years and 14 years, respectively. Among all the patients, 22 were under 30-year-old, 50 patients between 30-year-old and 50-year-old and 108 patients over 50-year-old. Seventy-nine patients (64.75%) with severe forms were over 50-year-old. For gender, there were more men than women in the severe form, i.e. 74 patients (60.65%) against 48 patients (39.35%).
In terms of occupation, traders accounted for the most in the total patients, followed by housewives and health workers. The most frequent comorbidities were Arterial Hypertension (HTA) (38.33%) and diabetes (18.88%). More than a quarter of patients with severe forms were hypertensive (36.88%), and 21.31% were diabetic. Clinically, cough (92.77%), dyspnea (80%) and fever (46.11%) were the most frequent signs. Other symptoms are shown in (Table 1).
Mean pulse oxygen saturation (SpO2) in room air was 88%. Most patients (81.11%) had a SpO2 below 93% (Table 1). 113 patients (91,86%) presented a normal respiratory rate (RR ≤ 30) while 8,13% had a higher rate (RR > 30). Some patients had a missing data on the respiratory rate.
Statistical Estimate
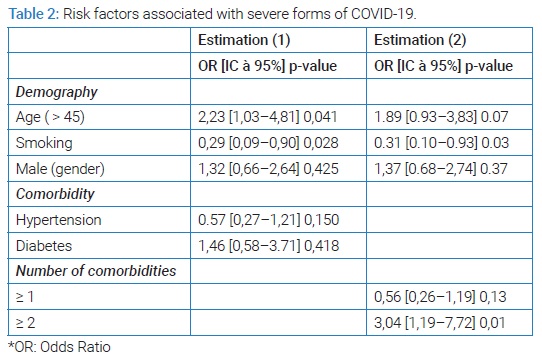
The odds-ratio for age and smoking is respectively 2.23 (p-value = 0.04) and 0.29 (p-value = 0.02) for the estimate (1). According to these results, advanced age is significantly associated with the severe form (OR > 1), while smoking was linked with the non-severe form (OR < 1). Among the significant variables, age has an odds-ratio value greater than 1, which indicates its strong association with the severe form of COVID-19. Gender, hypertension and diabetes are excluded from the association hypothesis since their p-value is greater than 5%. Nevertheless, the estimate (2) confirmed that the number of comorbidities greater than or equal to 2 is a factor linked to the severe form of COVID-19. The results of estimates (1) and (2) are presented in (Table 2).
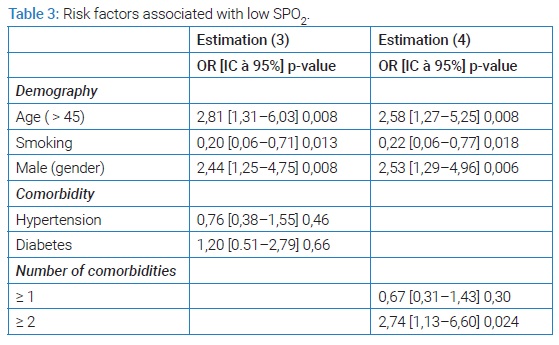
Later, we only consider SpO2, as a criterion of severity. Then, we establish the estimates (3) and (4) in which the dependent variable is the SpO2 in ambient air. The results are reported in (Table 3). Its difference from the result of the estimates (1) and (2) lies in the fact that gender has become statistically significant, that is, it has become one of the factors explaining the decrease in the value of SpO2 in ambient air. Advanced age and smoking remain significant.
Discussion
In this study, the data collected indicated that almost half of the patients (122) had a severe form. We found that advanced age and male gender are risk factors associated with the severe form while smoking is associated with the non-severe form. The impact of hypertension and diabetes on patients with COVID-19 has not been statistically validated.
Several studies have shown that the elderly eventually present with a severe form of COVID-19 [16,17]. In the United States, 95% of patients who died of COVID-19 were over 50-year-old [18]. For our study, the result showed that advanced age (45 years and older) influences the severity of COVID-19. This situation can be explained by the physiological changes that accompany aging and potential health problems. Takahashi et al. [19], had found in their studies the participation of the weakness of the immune system, the disorder of organic function, and the coexistence of comorbidities in subjects with advanced age. Compared to the association of a single comorbidity with the severe form of COVID-19, contrary to Wang et al. [14], our study failed to show this association. Hypertension and diabetes are not significantly associated with the severe form of SARS-CoV-2 infection. This result is similar with the work of Ouédraogo et al. [12], carried out at the University Hospital of Tingandogo (Burkina-Faso). However, our study showed that patients with at least two types of comorbidity (whatever they were) developed a severe form. Comorbidity studies revealed that after transmission of SARS CoV-2 in the human body, ACE-2 receptor or angiotensin-converting enzyme 2 accelerates the arrival of the virus to their target cells while patients with diabetes and hypertension contain a high value of ACE-2, which could cause the severity of SARS-CoV-2 infection [15,20].
The effect of smoking on the patient with COVID-19 has been discussed in the literature [21–24]. Being the cause of several respiratory and cardiovascular diseases, smoking is responsible for more than 8 million deaths worldwide [25]. Some studies have claimed that gene expression and subsequent receptor levels are elevated in the airways and oral epithelium of current smokers [26]. This could put smokers at a higher risk of contracting SARS-CoV-2. It is also known for the risk of viral and bacterial respiratory infections [27–29]. In addition, cigarette smoke reduces respiratory immune defense through peribronchiolar inflammation and fibrosis [30]. However, other studies have reported that nicotine down regulates the ACE-2 receptor. Smoking is thus considered a protector against COVID-19 [31,32]. The same result was found in our study concluding that smoking is a factor associated with the non-severe form of COVID-19. However, previous studies indicating the same association have been criticized for their biased results. For Cai [26], it is not appropriate to compare the prevalence of smoking in hospitalized patients with COVID-19 with estimates of the general population because of the intrinsic difference between the two populations in terms of demographic factors. Additionally, the World Health Organization (WHO) released a statement urging caution regarding claims about the link between smoking (or nicotine) and the prevention or treatment of COVID. -19. He pointed out the lack of evidence confirming this relationship [33].
Then, we showed that the male gender was likely to develop the risk of having a drop in SpO2 in ambient air, which is consistent with the result found in other studies conducted in France and China [34,35]. The high blood concentration of the Angiotensin-2 Converting Enzyme and the alteration of the immune system by androgens (testosterone, progesterone) in male subjects could explain this risk [36,37]. Expression of ACE-2 relies on the X chromosome, thus making males a potentially high express or of ACE-2. This facilitates the action of the virus to reach the target cell.
We encountered some limitations for this study. First, several paraclinical data such as laboratory characteristics and radiological signs were not complete during the processing of patient records. This could help us identify other factors influencing the state of health of a patient with COVID-19. For example, several studies speak of lymphopenia, which proves to be an important factor explaining the severity of COVID-19, whereas the data we have processed lack it. Then, the criterion used to qualify the severity of the infection could be insufficient. Bilateral lung involvement could have been used as a criterion but the data were insufficient. Finally, this article is essentially limited to the clinical manifestations presented by the patients.
Conclusion
The result showed that advanced age and male gender are risk factors associated with severe forms of COVID-19 while high blood pressure and diabetes were not statistically significant. Smoking is associated with the mild form of covid19. This should not lead anyone to think of smoking as a means of preventing or treating COVID-19. It only opens the discussion on the need for in-depth research on this subject.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
- Zhu N, Zhang D, Wang W, Xingwang L, Yang B, Jingdong S, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(2):727–733.
- Wu Y, Ho W, Huang Y, Dong-Yan J, Shiyue L, Shan-Lu L, et al. SARS-CoV-2 is an appropriate name for the new coronavirus. Lancet. 2020;395(10228):949–950.
- Lipsitch M, Swerdlow DL, Finelli L. Defining the epidemiology of Covid-19 - studies needed. N Engl J Med. 2020;382(13):1194–1196.
- Zhang Y, Wang J, Nannan T, Du K, Gao K, Zuo J, et al. Risk factors in patients with diabetes hospitalized for covid-19: findings from a multicenter retrospective study. J Diabetes Res. 2021;2021:3170190.
- Yuxin Y, Woo IS, Yoong XP, Yang M, Jianchen L, Chong Y, et al. The first 75 days of novel coronavirus (SARS-CoV-2) outbreak: recent advances, prevention, and treatment. Int J Environ Res Public Health. 2020;17(7):2323.
- Hozhabri H, Sparascio FP, Hamidreza S, Mousavifar L, Roy R, Scribano D, et al. The global emergency of novel coronavirus (SARS-CoV-2): an update of the current status and forecasting. Int J Environ Res Public Health. 2020;17(16):5648.
- Xu Z, Shi L, Wang Y, Zhang J, Huang L, Zhang C, et al. Pathological findings of covid-19 associated with acute respiratory distress syndrome. Lancet Respir Med. 2020;8(4):420–422.
- Zhou F, Yu T, Ronghui D, Guohui F, Ying L, Zhibo L, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062.
- Wu J, Li W, Shi X, Z Chen, B Jiang, Liu J, et al. Early antiviral treatment contributes to alleviate the severity and improve the prognosis of patients with novel coronavirus disease (COVID-19). J Intern Med. 2020;288(1):128–138.
- Shi Y, Yu X, Zhao H, Wang H, Zhao R, Jifang S, et al. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care. 2020;24(1):108.
- Ouédraogo AR, Bougma G, Baguiya A, Sawadogo A, Kaboré PR, Minougou CJ, et al. [Factors associated with the occurrence of acute respiratory distress and death in patients with COVID-19 in Burkina Faso]. Rev Mal Respir. 2021;38(3):240–248.
- Berlin DA, Gulick RM, Martinez FJ. Severe Covid-19. N Engl J Med. 2020;383(25):2451–260.
- Wang B, Li R, Lu Z, Huang Y. Does comorbidity increase the risk of patients with COVID-19: evidence from meta-analysis. Aging (Albany NY). 2020;12(7):6049–6057.
- Griffith G, Morris TT, Tudball M, Herbert A, Mancano G, Pike L, et al. Collider bias undermines our understanding of COVID-19 disease risk and severity. medRxiv. 2020.
- Abdulzahra H, Deepak R, Buttle T, Linkson L, Owen W, Hadley E, et al. Risk factors for severe coronavirus disease (COVID-19). EMJ Respir. 2020;8(1):120–126.
- Placais L, Richier Q. [COVID-19: Clinical, biological and radiological characteristics in adults, infants and pregnant women. An up-to-date review at the heart of the pandemic]. Rev Med Intern. 2020;41(5):308–318.
- Rachel N. Chronic conditions, aging immune systems increase vulnerability. Aarp. 2021.
- Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588(7837):315–320.
- Benowitz NL, Schultz KE, Haller CA, Wu AHB, Dains KM, Jacob P. Prevalence of smoking assessed biochemically in an urban public hospital: a rationale for routine cotinine screening. Am J Epidemiol. 2009;170(7):885–891.
- Vardavas CI, Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob Induc Dis. 2020;18:20.
- World Health Organization. Smoking and COVID-19. 2020. [https://www.who.int/news-room/commentaries/detail/smoking-and-covid-19]
- Simons D, Shahab L, Brown J, Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalisation and mortality from COVID-19: A living rapid evidence review with Bayesian meta-analyses (version 10). Qeios. 2021.
- Guan WJ, Zheng-Yi N, Yu H, Liang W, Ou C, Jian-xing H, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720.
- United States Public Health Service Office of the Surgeon General; National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health. Smoking Cessation: A Report of the Surgeon General [Internet]. Washington (DC): US Department of Health and Human Services; 2020.
- Cai G. Bulk and single-cell transcriptomics identify tobacco-use disparity in lung gene expression of ACE2, the receptor of 2019-nCov. MedRxiv. 2020.
- Abadom TR, Smith AD, Tempia S, Madhi SA, Cohen C, Cohen AL. Risk factors associated with hospitalisation for influenza-associated severe acute respiratory illness in South Africa: A case-population study. Vaccine. 2016;34(46):5649–5655.
- Feldman C, Anderson R. Cigarette smoking and mechanisms of susceptibility to infections of the respiratory tract and other organ systems. J Infect. 2013;67(3):169–184.
- Huttunen R, Heikkinen T, Syrjänen J. Smoking and the outcome of infection. J Intern Med. 2011;269(3):258–269.
- Dye JA, Adler KB. Effects of cigarette smoke on epithelial cells of the respiratory tract. Thorax. 1994;49(8):825–834.
- Farsalinos K, Barbouni A, Niaura R. Systematic review of the prevalence of current smoking among hospitalized COVID-19 patients in China: could nicotine be a therapeutic option? Intern Emerg Med. 2020;15(5):845–852.
- Oakes JM, Fuchs RM, Gardner JD, Lazartigues E, Yue X. Nicotine and the renin-angiotensin system. Am J Physiol Regul Integr Comp Physiol. 2018;315(5):R895–R906.
- World Health Organisation. WHO statement: tobacco use and COVID‐19. WHO. 2020. [https://www.who.int/news/item/11-05-2020-who-statement-tobacco-use-and-COVID-19]
- Jean-Guillaume B. Serious forms of Covid-19: a risk multiplied by three for men. Pourquoi docteur. 2021.
- Manelli S. The coronavirus would be more dangerous for men. La Provence. 2020.
- Klein SL, Flanagan KL. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–638.
- Biswas M, Rahaman S, Biswas TK, Zahirul H, Baharudin I. Association of sex, age, and comorbidities with mortality in covid-19 patients: a systematic review and meta-analysis. Intervirology. 2020;1–12.
Keywords
COVID-19; Risk factors; SARS CoV-2; Severe form
Cite this article
Razafimpihanina SM, Ramandray F, Rasoafaranirina MO, Rakotondrabe DI, Razafindrasoa AZ, Andriarimanga DO, et al. Risk factors associated with the appearance of the severe form of COVID-19 in the pulmonology departments of Antananarivo, Madagascar. World J Public Health Epidemiol. 2022;1(2):1–6.
Copyright
© 2022 Razafimpihanina Sonia Marcelle. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).