Abstract
Granuloma gravidarum is a tumor-like inflammatory lesion presenting as a painless, vascular granulation tissue with a rapid course of enlargement, developing during pregnancy. An exaggerated response to local irritants caused by high levels of estrogen and progesterone hormones is the pathogenic aspect of granuloma gravidarum. Although it may regress spontaneously after childbirth, it may also be persistent in the postpartum period. In cases where this lesion reaches an increased size, difficulty in mastication, speaking, and mouth closure might occur. We report two female patients with enlarged granuloma gravidarum lesions creating interference with mastication along with their clinical and histopathological findings. Surgical excisional biopsy was performed in both patients under local anesthesia and oral hygiene was improved. Management of granuloma gravidarum is important during pregnancy, considering that overgrown lesions may affect nutrition and therefore a healthy pregnancy period.
Abbreviations
Basic Fibroblast Growth factor (bFGF); Hematoxylin and Eosin (H&E); Interleukin-1 beta (IL-1β); Scaling and Root Planning (SRP); Tumor Necrosis Factor-alpha (TNF-α); Vascular Endothelial Growth Factor (VEGF)
Introduction
Granuloma gravidarum is an inflammatory lesion characterized by a painless, vascular granulation tissue developing during the pregnancy [1,2]. It clinically presents as a pedunculated or sessile; pink, red, or purple-colored lesion with a bleeding tendency, usually occurring in the anterior and buccal regions of the maxilla [1]. Although it has been stated by various names such as granuloma gravidarum, pyogenic granuloma, or pregnancy tumor, the histopathological aspect of this lesion is the same as that of pyogenic granuloma in which vascular proliferation and inflammatory cells are observed [2–4]. However, when the lesion develops due to hormonal alterations during pregnancy, it is diagnosed as granuloma gravidarum [3]. The incidence of granuloma gravidarum in pregnant women has been reported as 0.5%–5% [1]. Poor oral hygiene, persistent bacterial plaque, local irritation, and oxidative stress have been stated as predisposing factors associated with the development of this reactive tissue growth [3]. Even though the lesion may regress spontaneously following childbirth, surgical excision is recommended in some cases in the postpartum period, and plaque control is important to prevent recurrences [1,2]. In addition, it has been suggested that the use of antioxidant supplements may also affect the treatment process of maternal periodontal diseases by reducing oxidative stress [5]. Healthy diet including fruits and vegetables, can supply the body with beneficial nutrients and antioxidants including coenzyme Q10 and alpha-tocopherol which have a neuroprotective as they proved to have protective effects of antioxidants [6,7]. Surgical intervention during pregnancy should only be considered when there is a difficulty in mastication or an aesthetic concern [2]. In this article, two female patients with overgrown granuloma gravidarum lesions creating interference with mastication are presented along with their clinical and histopathological findings.
Case Presentation
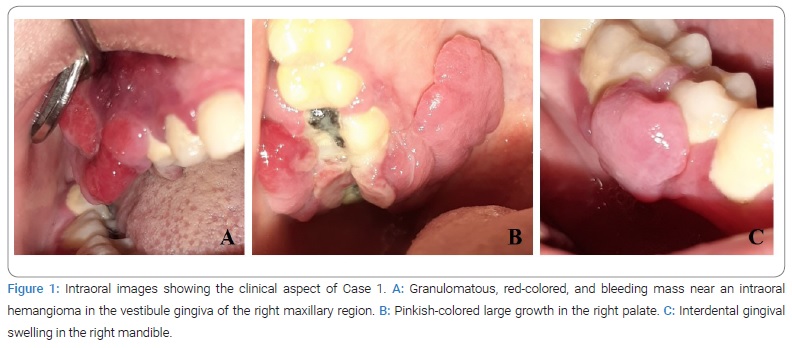
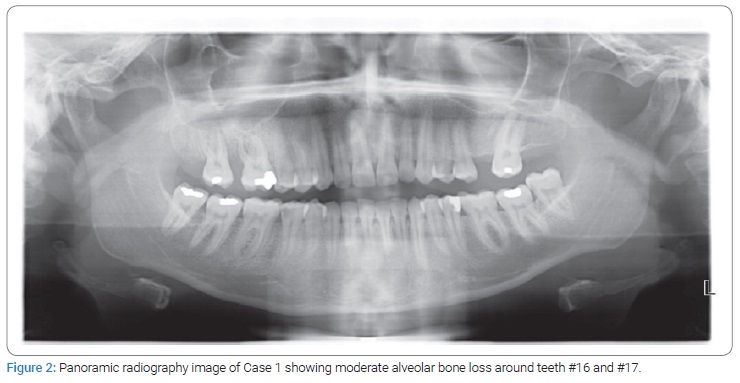
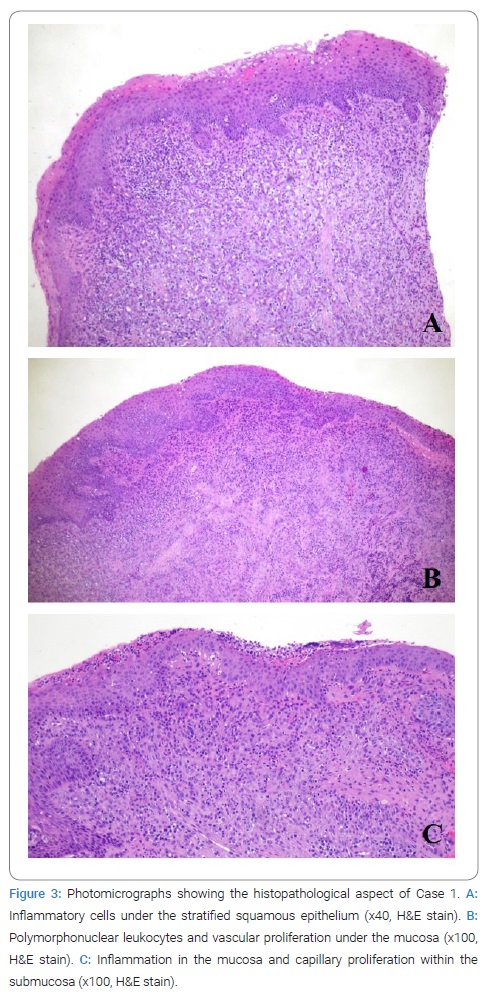
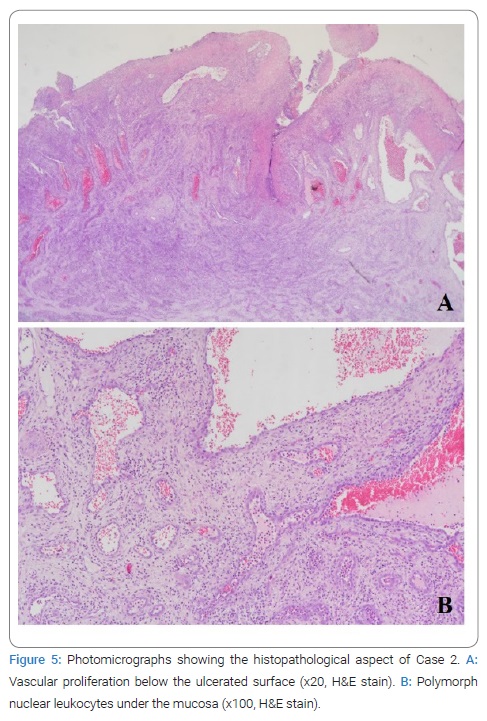
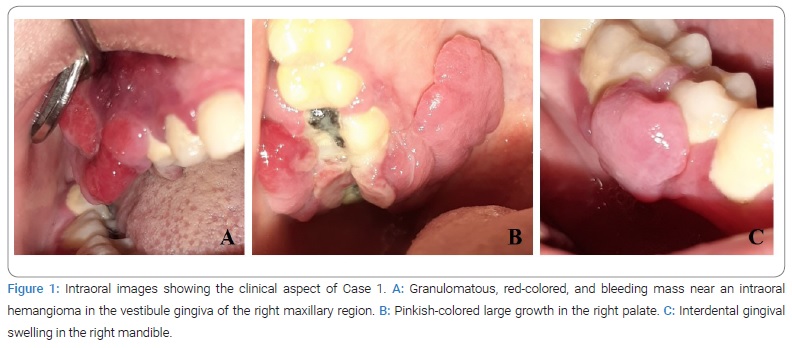
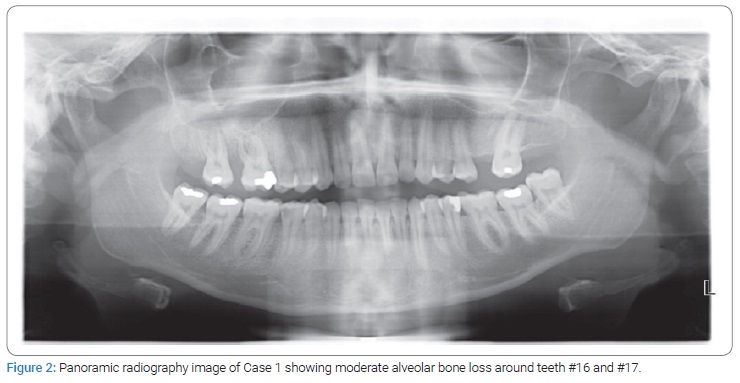
Case 1: A 27-year-old female patient presented to the Department of Oral and Maxillofacial Radiology with complaints of painless and hemorrhagic gingival and mucosal swellings in the right maxillary region, palate, and right mandibular region. The duration time of the lesions was more than one year. The medical anamnesis revealed a past pregnancy that ended in birth seven months ago, and the patient reported that it was her first pregnancy. The patient also stated the lesions had appeared in the 2nd month of the pregnancy and progressively increased in size throughout the pregnancy. No medication use or comorbidity, other than poor oral hygiene, were detected which may be associated with the development of the lesion. The intraoral examination disclosed a granulomatous, red-colored lesion with a severe bleeding tendency, and an intraoral hemangioma in the vestibule gingiva of the right maxillary region. Additionally, a large pinkish-colored growth in the right palate and interdental gingival swelling in the right mandibular region were detected (Figure 1). Radiographic examination with a panoramic image showed moderate alveolar bone loss around teeth #16 and #17 (Figure 2). The patient was referred to the Department of Oral and Maxillofacial Surgery for the surgical excision of the lesions along with extraction of teeth #17 under local anesthesia, and a biopsy was suggested. Surgical treatment was put in front of periodontal treatment because of the great decrease in chewing function. Histopathological examination performed under Hematoxylin and Eosin (H&E) staining disclosed inflammatory cells, polymorph nuclear leukocytes and capillary proliferation (Figure 3). In accordance with this, the biopsy result was pyogenic granuloma. Due to patient’s past pregnancy, lesions were diagnosed as granuloma gravidarum. Oral hygiene was maintained after surgical excision and no recurrence was detected in the 3rd month follow-up.
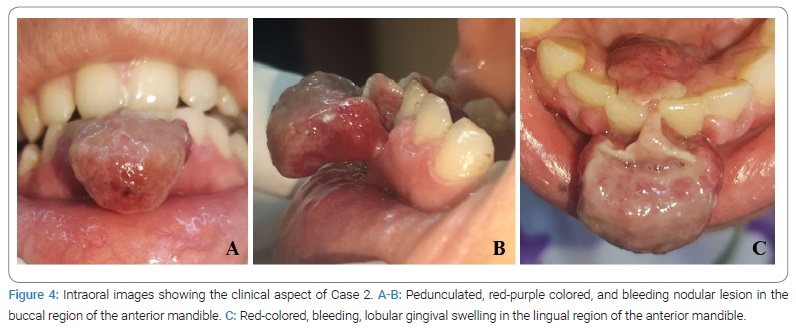
Case 2: A 34-year-old female patient with a seven-month first pregnancy was referred to our department for gingival swellings with a bleeding tendency in the anterior mandibular region and difficulty in mastication. The patient reported that the lesions had been present for one month and had a rapid course of enlargement. In the medical anamnesis, no disease or drug use related to the progression of the lesions was detected. However, the patient had a lack of oral hygiene. Intraoral examination revealed a pedunculated, red-purple colored, nodular lesion and a red-colored, bleeding, lobular gingival swelling in the buccal and lingual regions of the anterior mandible, respectively (Figure 4). Radiographic examination could not be performed because of the current pregnancy of the patient.
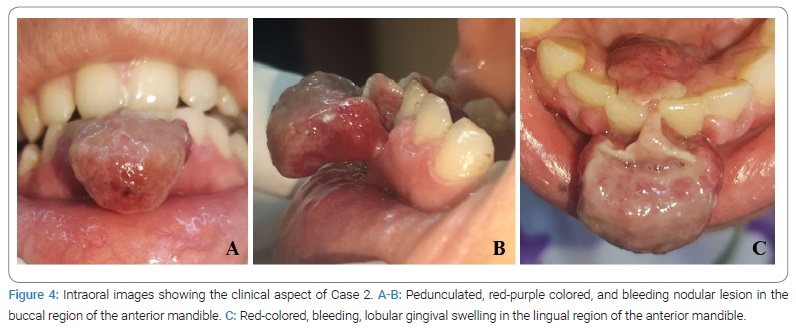
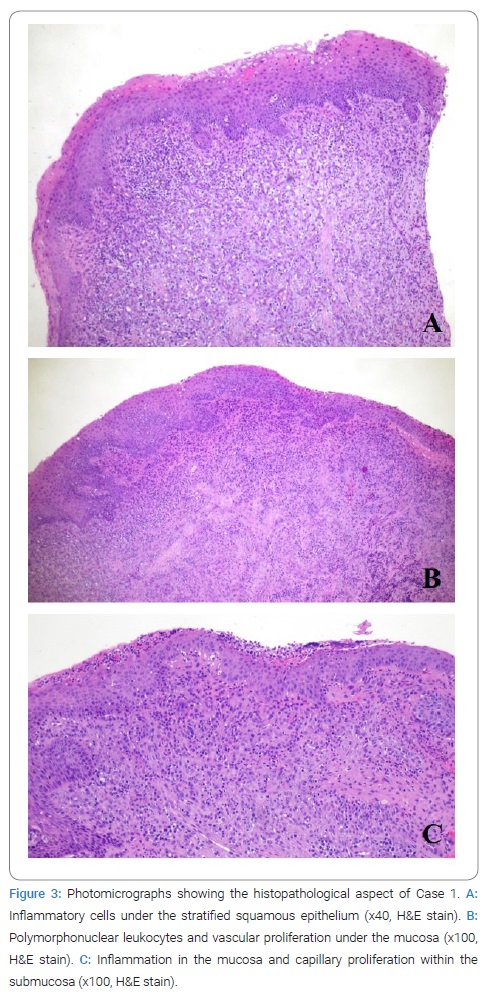
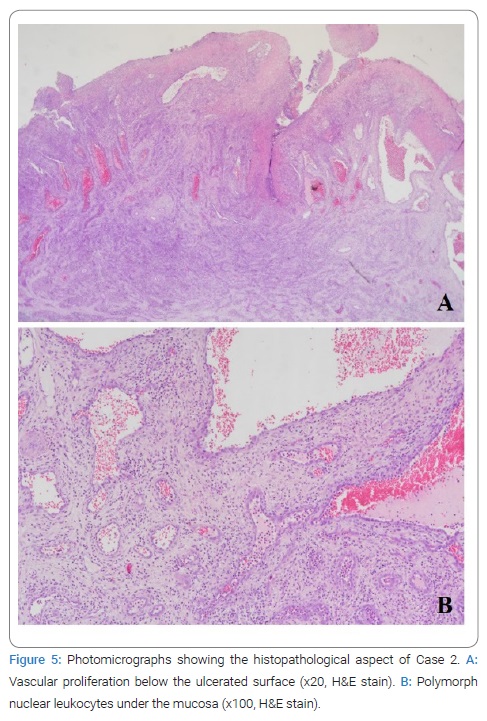
Excision of the buccal lesion under local anesthesia was recommended before the periodontal treatment due to the patient’s current pregnancy and limited mastication and mouth closing. Following consultation with the patient’s gynecologist, and obtaining permission, a surgical excision under local anesthesia was performed. Surgical treatment of the lingual lesion was postponed until the end of the pregnancy after maintaining plaque control. Histopathological examination with H&E stained sections revealed vascular proliferation and polymorph nuclear leukocytes below the ulcerated surface (Figure 5). Due to histopathological aspect of the lesion, the final diagnosis was determined as granuloma gravidarum.
Discussion
Granuloma gravidarum is a reactive tumor-like proliferation caused by an exaggerated response of periodontal tissues to local irritants resulting from hormonal changes during pregnancy [4]. It has been suggested that the increased levels of estrogen and progesterone hormones play an important role in pathogenesis by stimulating the overexpression of angiogenic factors such as Vascular Endothelial Growth Factor (VEGF) and Basic Fibroblast Growth Factor (bFGF) [8]. Due to high levels of female steroid hormones during the pregnancy, exacerbated inflammatory response may occur in the periodontium resulting from the altered vascular response and connective tissue turn-over [1]. Furthermore, down-regulation of cytokines such as interleukin-1 beta (IL-1β) and Tumor Necrosis Factor-alpha (TNF-α) because of increased estrogen and progesterone may prevent the apoptosis of granuloma cells in pregnant patients [8,9]. Aside from the angiogenic and inflammatory mechanisms, pregnancy-related periodontal disease has been reported to be associated with increased oxidative stress during pregnancy, which may predispose to the development of granuloma gravidarum [9]. Along with the above mentioned mechanisms, poor oral hygiene, trauma, and local irritating factors like bacterial plaque, calculus, or foreign materials are also considered as important risk factors for the development of granuloma gravidarum [2,3]. There are different opinions about the development time of granuloma gravidarum. Jafarzadeh et al. [3] stated that it generally appears in the 2nd month and 3rd month of pregnancy. However, according to Cardoso et al. [2], women up to the age of 25 tend to develop this lesion in the 1st trimester, whereas women aged 26 years–35 years in the 3rd trimester. We reported a 27-year-old patient who developed granuloma gravidarum in the 1st trimester, and a 34-year-old patient at the end of the 2nd trimester, which was comparable with the findings of Cardoso et al. [2] In this respect, it is of great importance to follow-up the patients and control bacterial plaque throughout the whole pregnancy period, as well as raising the awareness of the patients in order to prevent the development of granuloma gravidarum. Granuloma gravidarum predominantly occurs on the gingiva and rarely on the tongue, lips, palate and buccal mucosa [2]. We presented a palatal lesion originating from the gingiva and enlarged through the palatal region in Case 1. Since it is a rare localization, there is a limited number of studies reporting palatal granuloma gravidarum [4,10]. Therefore, we believe that our case has contributed to the literature in this direction. To our knowledge, there are different studies presenting other rare placements like tongue [11] and extra-orally areas such as nasal fossa [12]. Even though the above-mentioned cases provide important contributions as well, the lesion sizes reported in our case were also noteworthy, since such large soft tissue growths should be differentiated from malignancy. Therefore, histopathological examination is crucial to determine the final diagnosis. Differential diagnosis of granuloma gravidarum should include peripheral giant cell granuloma, peripheral ossifying fibroma, hemangioma, metastatic tumor, Kaposi sarcoma, angiosarcoma, and non-Hodgkin’s lymphoma [3,4,13]. Scaling and Root Planning (SRP) is the gold standard non-surgical therapy for periodontitis, and systemically administered antibiotics can be used as an adjunct to SRP to improve the treatment outcome of periodontitis [14]. In the case of granuloma gravidarum, the treatment procedure depends on its clinical presentation and the severity of the patient’s complaints [3]. Some small lesions may regress by eliminating local irritants or spontaneously after childbirth [1,2]. However, persistent enlarged lesions in the postpartum period have been reported by many authors, including our study as well [4,13]. Surgical intervention is indicated for such lesions, and improved oral hygiene is essential in order to prevent recurrences [1]. Surgical excision is the most preferred treatment protocol for large lesions, however, varied alternative techniques such as Nd:YAG laser, CO2 laser, flash lamp pulsed dye laser, cryosurgery, absolute ethanol injection, and corticosteroid injection have also been proposed by different authors [3]. The use of Nd:YAG laser may be beneficial in cases with a high risk of bleeding, as in our Case 1 where a granuloma gravidarum developed very close to an intraoral hemangioma. Intralesional corticosteroid injections might be considered for lesions with a high risk of recurrence [3].
Management of granuloma gravidarum during pregnancy is important, because overgrown lesions may cause halitosis, or difficulty in chewing and speaking [10]. Removing bacterial plaque, maintaining oral hygiene and preferring soft toothbrushes are recommended to prevent development of granuloma gravidarum or control the size of the already developed lesions [3]. Patient education also plays a critical role in terms of the prognosis of treatment and prevention of recurrences. Abou El-Fadl et al. [14] Reported that the clinical results for the patients who received patient education were more promising than those of patients who received periodontal treatment only. Even though the use of oxidative supplements has been thought to be beneficial in the management of the maternal periodontal disease [5], Ardalic et al. [15] showed that there was not any significant difference regarding oxidative stress in pregnant patients who took and did not take antioxidant supplements. Surgical treatment should be postponed until the postpartum period [3]. However, when there is a major difficulty in mastication, surgical intervention during pregnancy should be considered and if it is necessary, should be performed in the 2nd trimester [2]. In both of our cases, surgical excision under local anesthesia was preferred. Even though our Case 2 was in the 3rd trimester, it was decided to perform surgical intervention due to the major difficulty in mastication as mentioned above. Recurrence and the need for re-excision might occur in 16% of the cases due to poor oral hygiene, inadequate surgery, or recurrent trauma [3]. Therefore, eliminating bacterial plaque and regular follow-up appointments after delivery are critical to ensure healing, as well as to prevent re-development of lesions [2]. In our report, no recurrence was observed in Case 1, pointing out the importance of maintaining oral hygiene after excision. In this study, two granuloma gravidarum cases, which interfered with mastication, and reduced the quality of life, were defined, emphasizing the importance of managing overgrown inflammatory lesions in pregnant patients, which is the strength of our case report. However, the small number of cases and lack of long-term follow-up after delivery may be considered as the weaknesses of the study. Further studies with larger patient groups along with longer follow-up periods will be enlightening in revealing the importance of overgrown granuloma gravidarum lesions preventing function in pregnancy. Moreover, to make a criticism of our treatment technique, even though we postponed the periodontal treatment until after the surgical intervention due to the clinical conditions and urgencies of the patients, pre-surgical periodontal treatment is recommended to improve the treatment outcome and provide a better prognosis in the postoperative period.
Conclusion
It is possible to encounter Granuloma Gravidarum type inflammatory lesions with the predisposing effect of changes in hormonal conditions related to pregnancy on the oral cavity. It is essential to avoid and manage granuloma gravidarum, since overgrown lesions may affect a healthy pregnancy period. Eliminating local irritants by pre-surgical periodontal treatment is an important part of the treatment process of granuloma gravidarum. However, surgical intervention may be required for large lesions. We reported two overgrown granuloma gravidarum lesions which were managed by excisional surgery and oral health improvement. Periodontal treatment was postponed until after the surgery due to urgent conditions of the patients, and major reduce in their quality of life. The importance of histopathological evaluation and patient history should also not be overlooked, considering that such large soft tissue lesions can easily be confused with malignancy.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
Keywords
Granuloma gravidarum; Palate; Pregnancy tumor; Postpartum period; Pyogenic granuloma
Cite this article
Aslan E, Elgün F, Dündar N, Mızrak A, Yaman B. Granuloma Gravidarum preventing mastication: report of two cases. Glob J Oral Maxillofac Surg. 2023;1(1):1–6.
Copyright
© 2023 Elif Aslan. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).