Abstract
Introduction: Sarcoidosis is a rare idiopathic systemic inflammatory disease that mainly affects the lymph nodes, lungs, skin and eyes. Nervous system involvement is only seen in 5% of cases of sarcoidosis. Cerebral vasculitis, is particularly uncommon in patients with sarcoidosis, with serious outcome.
Case report: We reported the case of a 55-year-old female who developed a severe hemicranial headache with nausea and vomiting. She had a history of erythema nodosum. The clinical examination showed left arm weakness and central facial paralysis, along with arthralgia. Brain MRI revealed a moderate subarachnoid hemorrhage, multiple acute lacunar infarcts, and a large ischemic stroke over the right middle cerebral artery territory; and MR angiography revealed a Moya-Moya like vasculopathy pattern and the occlusion of intracranial internal carotid arteries. Findings in the CT chest and abdomen scan, and Broncho alveolar lavage confirmed the diagnosis of sarcoidosis.
Conclusions: Cerebrovascular manifestations are uncommon in sarcoidosis. Multiple factors seem to be involved in the pathogenesis of sarcoidosis related vasculopathy. The diagnosis should be considered when recurrent infarcts and hemorrhage are encountered in a patient having systemic symptoms of sarcoidosis.
Introduction
Sarcoidosis is a rare idiopathic systemic inflammatory disease characterized by the formation of noncaseating granulomas. It most commonly affects the lymph nodes, lungs, skin and eyes. Nervous system involvement is only seen in 5% of cases of sarcoidosis [1,2]. Neurologic manifestations usually include cranial neuropathies, aseptic meningitis, myelopathy, hydrocephalus and intraparenchymal mass lesions [1,2]. Cerebrovascular involvement, specifically cerebral vasculitis, is a rare occurrence in sarcoidosis with a high risk of morbidity and mortality.
Here, we report an uncommon case of cerebral Moya-Moya-like vasculopathy as a presentation of Neuro-Sarcoidosis (NS) in a patient with a systemic sarcoidosis.
Case Presentation
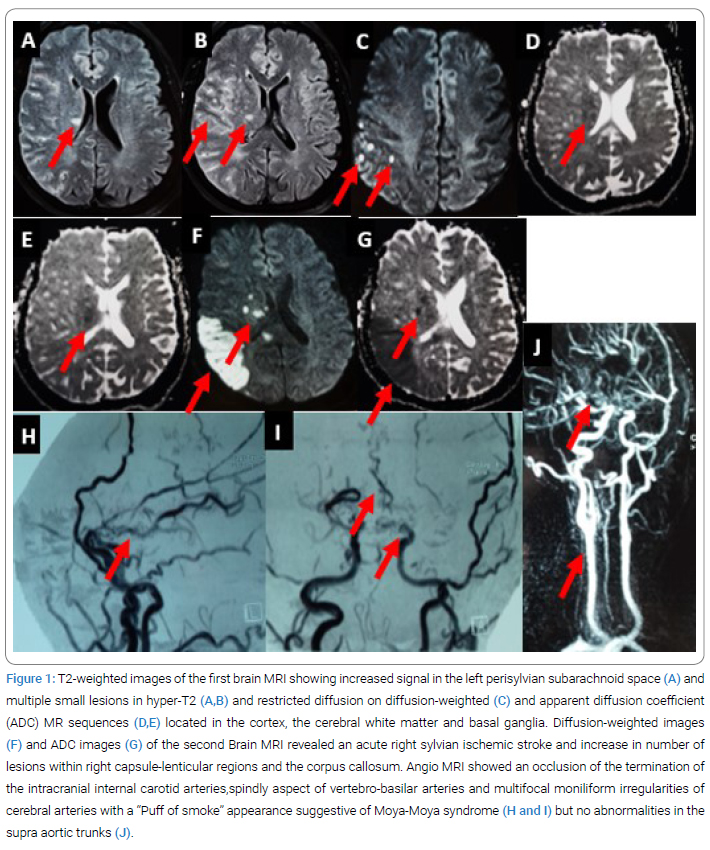
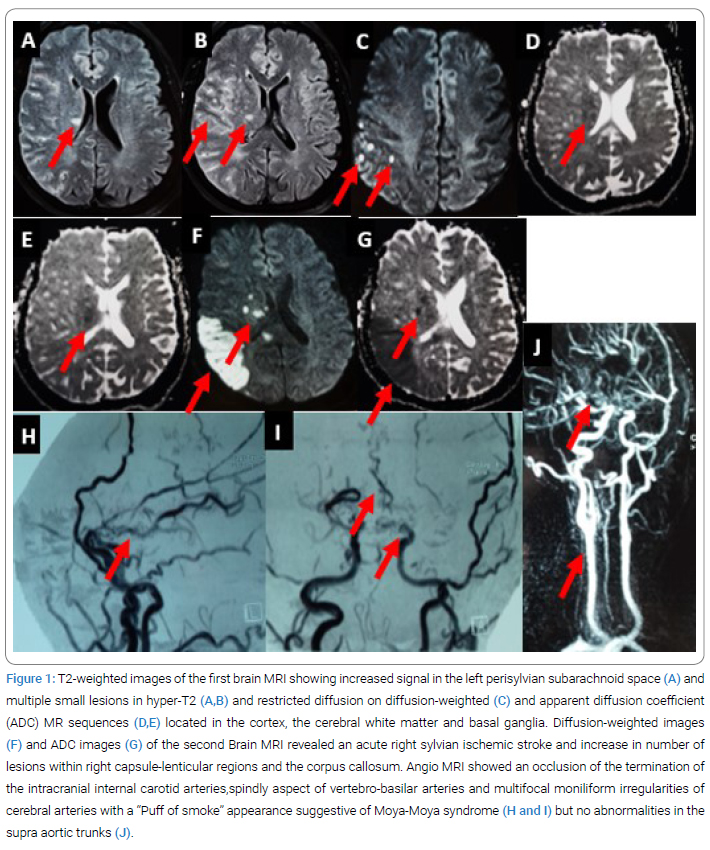
A 55-year-old right-handed female presented with an acute onset headache for the past 2 days. This headache was described as sudden severe right hemicranial headache accompanied by nausea and vomiting. The patient had a history of erythema nodosum. No history of head trauma or family history of stroke or migraine was found. On arrival, she was conscious and oriented. Her neurological examination was normal except for brisk tendon reflexes. She had no fever, nor neck stiffness, nor skin lesions, nor visual disturbances. However, she was complaining from join pain over both ankles without arthritis. Brain MRI showed abnormal signal (increased in T2-FLAIR and decreased in T2* weighted images) in the subarachnoid space, especially in the right hemisphere and the right Sylvian fissure, consistent with moderate subarachnoid hemorrhage. Besides, multiple small hyper T2 lesions in the right fronto-parieto-occipital regions, the right thalamus and internal capsule. These lesions showed restricted diffusion on diffusion-weighted and apparent diffusion coefficient MR sequences suggestive of lacunar infarcts (Figure 1A,1B,1C,1D and 1E). Angio MR showed an occlusion of the termination of the intracranial internal carotid arteries that extends to the proximal segments of the middle and anterior cerebral arteries, spindly aspect of vertebro-basilar arteries and multifocal moniliform irregularities within cerebral arteries associated to “Puff of smoke” appearance of an abnormal arterial supply mesh. These imaging findings were indicative of Moya-Moya disease, likely secondary to a vasculitis of brain vessels (Figure 1H and 1I). Echography and angio MR of the supra-aortic trunks showed no signs of vasculitis (Figure 1J).
Extensive laboratory investigation, including infectious serologies (hepatitis C and B, varicella, herpes simplex and Human Immunodeficiency Virus (HIV)), tuberculosis screening and serum protein electrophoresis was unremarkable. Vasculitis screen including antinuclear antibodies, anti-phospholipid antibodies, both P and C antineutrophil cytoplasmic antibodies and lupus anticoagulant, was negative. Angiotensin-Converting Enzyme (ACE) levels in serum and Cerebrospinal Fluid (CSF) were within normal ranges. Contrast-enhanced CT Chest, Abdomen and Pelvis (CAP) scan was normal. Eye examination showed no signs of vasculitis or uveitis, and the cardiac echography was normal.
Because of the history of erythema nodosum and the radiological aspect of cerebral vasculitis in the Brain MRI, a Broncho Alveolar Lavage (BAL) was carried out, revealing a mildly elevated cell count (31х104/ml) with lymphocytosis (45.2%), a high level of neutrophils (4.4%) and a normal percentage of alveolar macrophages and eosinophils (50.2% and 0.2% respectively). The CD4/CD8 ratio was elevated [3,7] and there were no hemosiderin-laden macrophages.
At this stage, the diagnosis of CNS vasculitis secondary to sarcoidosis was highly suspected. Eventually, the patient was started on 5 doses of one-gram intravenous methylprednisolone. Five days later, the headache progressively settled, but she experienced sudden onset of brutal weakness of her left arm and slight central facial paralysis without nausea nor vomiting (NIHSS score = 3). Urgent MRI was performed, demonstrating an acute ischemic stroke in the right middle cerebral artery territory and increase in number of lesions mainly within the distal territory of the middle cerebral artery, the right capsule-lenticular regions, the corpus callosum and parieto-occipital regions (Figure 1F and 1G). The patient was immediately started with high doses of oral steroids (1 mg/kg/day) along with azathioprine (3 mg/kg/day).
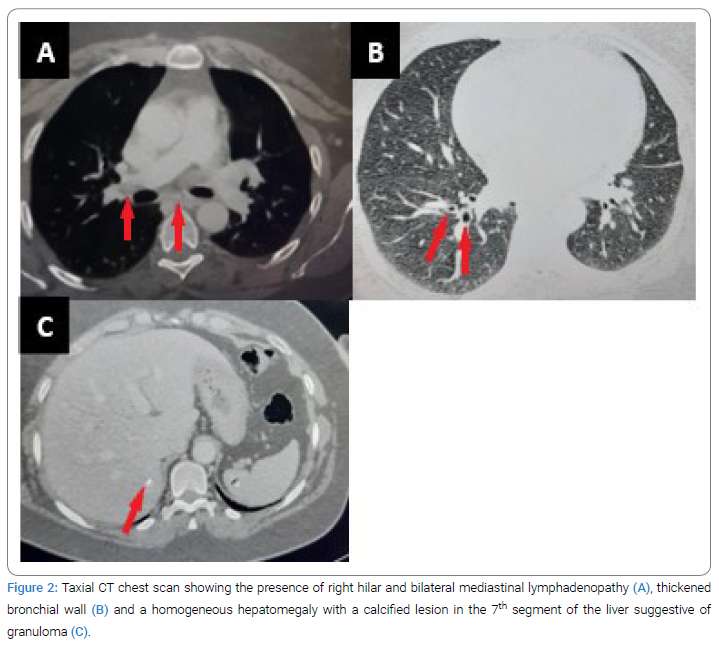
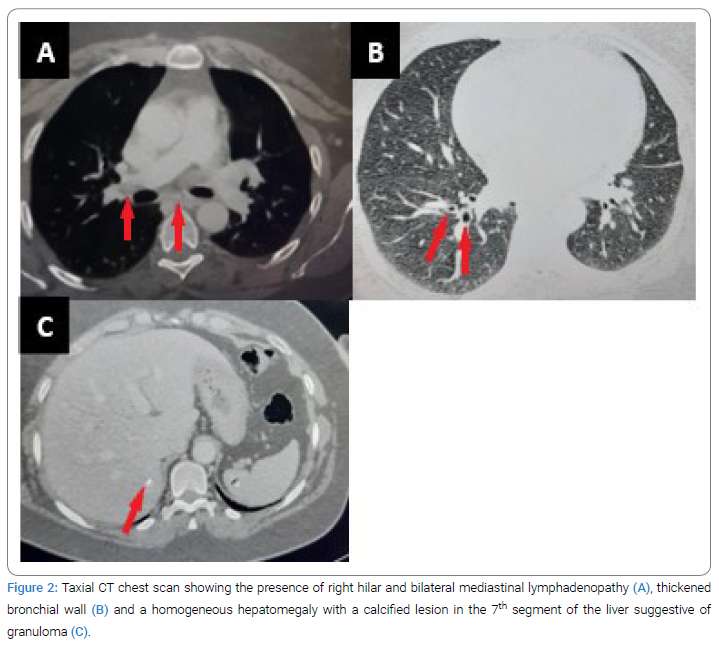
Three months apart from the neurological episode, CSF studies showed clear CSF, 10 white blood cells, slightly elevated protein (0.54 g/l), normal glucose levels (0.6 g/l) and no neoplastic cells. Multiple oligoclonal bands of specific Immunoglobulin G (IgG) were found in the CSF, with a high index of IgG (0.82) and an alteration of the blood-brain barrier (albumin quotient = 12.95). Another CT CAP scan was performed, indicating the presence of right hilar and bilateral mediastinal lymphadenopathy, as well as a homogeneous hepatomegaly with a lesion in the 7th segment of the liver suggestive of calcified granuloma (Figure 2A,2B,2C). However, the patient refused the biopsy of the lymph nodes.
At one-year follow-up, under 10 mg of corticosteroids and azathioprine (3 mg/kg/day), the patient did not have any motor deficit (NIHSS score = 0) and did not experience any recurrence of headaches, nor vascular cerebral episodes, nor respiratory symptoms, nor skin lesions.
Discussion
We presented a patient who developed acute headache, revealing a sarcoidosis related vasculitis. Because no lymph nodes biopsy was performed, this patient fulfilled the diagnostic criteria of possible NS outlined by the NS Consortium Consensus Group [3], as she developed clinical and radiological signs of a cerebral vasculitis, with few nonspecific signs of inflammation in the CSF study, along with systemic symptoms suggestive of sarcoidosis (erythema nodosum and polyarthralgia) and bilateral mediastinal adenopathy on CT scan. Abnormalities in the BAL were also suggestive of sarcoidosis, as a mildly elevated total cell count with a predominance of lymphocytes (15% to 50%), a normal percentage of eosinophils (≤1%), an increased level of neutrophils and lack of plasma cells and “foamy” alveolar macrophages is characteristic for sarcoidosis [4]. Likewise, the absence of hemosiderin-laden macrophages is particularly seen in sarcoidosis. In fact, it helps differentiate sarcoidosis from other types of vasculitis that can be associated with alveolar hemorrhage syndromes, especially Wegener’s granulomatosis [4]. Eventually, it was the CD4/CD8 ratio that was able to adjust the diagnosis, as it is highly specific of sarcoidosis when it is over 3.5.
The diagnosis of sarcoidosis related vasculitis was quite challenging, especially in the absence of pathology confirmation of granulomatosis disease. Rigorous investigation was needed in order to rule out all the differential diagnoses mainly infectious diseases like HIV, hepatitis, varicella, herpes simplex virus and tuberculosis, and autoimmune diseases such as Behçet disease, lupus, Wegener disease and polyarthritis nodosa [5]. Malignant neoplasms were also excluded through the absence of neoplastic cells on CSF study, absence of neoplasm on CT CAP scan and normality of serum protein electrophoresis. The Reversible Vasoconstriction Syndrome (RVS) was also suspected in this case, as the clinical presentation (thunderclap-like headache, stroke and subarachnoid hemorrhage) could be consistent with RVS. Although no follow-up imaging was performed, the presence of inflammation signs in the CSF study, and affected intracranial carotid arteries is unlikely seen in RVS. Furthermore, RVS brain imaging is generally normal or showing PRES-like lesions [6]. In this case, Brain MRI is showing multiple lacunar infarcts suggestive of vasculitis which consequently excluded the RVS diagnosis. Hematological disorders were also discussed mainly because they represent the most frequent etiology of cerebral infarct of unusual cause in young adults with 1% of cerebral infarction and 1% of hemorrhagic stroke [7]. We especially considered the diagnosis of Sickle-cell anemia, Polycythemia Vera and Essential Thrombocythemia as the patient developed both ischemic stroke and hemorrhagic complication. But since there was no history of vaso-occlusive crisis, the complete blood count was normal and the Brain MRI showed signs of cerebral vasculitis which ruled out the diagnosis of hematological disorders.
Although rare, vasculitis mainly due to autoimmune diseases such as Behçet disease, lupus, Wegener disease, sarcoidosis and polyarthritis nodosa were considered. In fact, according to Arboix et al. [8], ischemic stroke secondary to primary inflammatory vascular conditions was observed in only 6 of 70 patients with ischemic stroke of unusual cause. But because the patient had systemic symptoms suggestive of sarcoidosis and brain MRI relevant with inflammatory vascular changes, the diagnosis of sarcoidosis related vasculitis was highly suspected.
Cerebrovascular manifestations such as hemorrhage and stroke are uncommon in patients with sarcoidosis [5]. In fact, ischemic infarcts are rare, generally due to small-vessel vasculitis, but sometimes secondary to large-vessel inflammation or cardio embolism from sarcoid cardiomyopathy [5,9]. These ischemic strokes are often small affecting basal ganglia, thalamus and brain stem rather than superficial and subcortical white matter, as the perforating arteries are the most involved. They can be symptomatic, transient or even silent, only discovered through diffusion-weighted images [5,9]. Large-vessel strokes in sarcoidosis due to large vessel inflammation are exceptionally rare. In such cases, MRA can show large vessel stenosis or occlusion [5,9]. Hemorrhagic infarcts are also rare, with an incidence of 0.6% among patients with NS [10]. These lesions are predominately intraparenchymal and more likely supra-tentorial, but they rarely present with subarachnoid hemorrhage [11,12].
Because vasculitis is the common underlying etiology, both ischemic lesions and hemorrhage can be seen in the same patient at different point time [5]. Indeed, our patient developed subarachnoid hemorrhage and multiple ischemic strokes both small and large-vessel infarcts at the same period of time. Brain imaging guided the diagnosis, as MRI showed a moderate subarachnoid hemorrhage, multiple acute lacunar infarcts, and a large ischemic stroke over the right superficial Sylvian territory; and MR angiography revealed a Moya-Moya like vasculopathy pattern and the occlusion of intracranial internal carotid arteries.
CNS sarcoid vasculitis is not frequent, first described in 1974 by Lawrence PW et al. [13], since then, few cases were reported in the literature. According to Pawate et al. [14], study among 54 patients with NS, only one patient had an extensive brainstem and thalamic infarction caused by sarcoid vasculitis. Recently, Saygin et al. [15] had reported 25 NS patients having CNS vasculitis confirmed through biopsy or positive angiography and inflammatory CSF pattern.
CNS vasculitis can occur during the disease course of a systemic sarcoidosis [16,17], or revealing the disease [18,19]. Most of NS patients with cerebrovascular symptoms were not investigated for a cerebral vasculitis through high-resolution vascular imaging or brain biopsy. In 2021, Bathla G et al. [20] evaluated 13 NS patients, using vessel wall imaging and brain biopsy. Among them, 9 patients had vascular abnormalities in the vessel wall imaging and 5 had perivascular granulomas with vessel wall involvement in the brain biopsy while only 3 patients developed clinical cerebrovascular symptoms. Therefore, the involvement of intracranial vessel in NS is more frequent than previously considered.
Regarding the association between Moya-Moya vasculopathy and sarcoidosis, namely Moya-Moya like vasculopathy, it has been previously described in few cases [21–24]. However, due to the lack of large population-based multicentric studies, sarcoidosis is not recognized as a common Moya-Moya syndrome associated disease and the actual link is yet unclear [25]. Nevertheless, some autoimmune diseases, such as Graves’ disease, antiphospholipid antibody syndrome, systemic lupus erythematosus and vasculitis were lately reported to be associated with a Moya-Moya vasculopathy. This would support the hypothesis of a possible inflammatory mechanism [26].
In our case, the hypothesis of a Moya-Moya like vasculopathy related to sarcoidosis seems to be more plausible than a fortuitous association between Moya-Moya disease and sarcoidosis, as angiographic findings show a less pronounced Moya-Moya vessel development in our patient than seen in the authentic “puff of smoke” appearance of a Moya-Moya disease, and the presence of irregular shaped stenosis typically seen in vasculitis. Furthermore, there are evidence of inflammation in the CSF study [25]. Although no brain biopsy confirming the presence of non-necrotizing granulomatous inflammation was performed, the vessel wall imaging would have a great importance, in order to confirm the diagnosis of vasculitis in this case. In fact, the vessel wall imaging shows a circumferential wall enhancement suggestive of vascular inflammatory process [20].
The pathophysiology of cerebrovascular manifestation in sarcoidosis is still unclear, as according to some studies, it is not only the vessel wall infiltration that causes this vasculopathy. Recently, it has been shown that patients with sarcoidosis also have impaired endothelial function and elevated arterial stiffness [27]. Additionally to expanded endothelial damage, significantly increased CNS endothelial immunoglobulin G binding and elevated levels of endothelin-1 were found in patients with NS [5,28]. Thus, sarcoidosis related vasculopathy seems to be multifactorial rather than monocausal pathology. In our patient, small-vessel ischemic infarcts seem to be secondary to granulomas causing perivascular inflammation and infiltration. While, the most plausible mechanism for large vessel occlusion causing the right mild cerebral artery infarction is the invasion of endothelial wall leading to in situ thrombosis. The possibility of a cardiac embolism or an artery-to-artery embolism are unlikely, as angio MR of the supra-aortic trunks was normal and cardiac echography showed no signs of sarcoid cardiomyopathy.
Treatment of NS is based on corticosteroids associated to immunosuppressive therapies. Corticosteroids are widely considered to be first-line therapy for NS. Patients with severe presentations like our patient, require pulse-dose IV methylprednisolone, 1 g daily for 3 days to 5 days followed by a prolonged oral glucocorticoid taper [29]. The immunosuppressive therapy should generally be given to patients with NS with moderate to severe presentations [29]. Such aggressive protocols are necessary in sarcoidosis with cerebrovascular involvement, in order to limit the inflammation, prevent the occurrence of other cerebrovascular lesions, reduce the risk of morbidity and mortality, and ensure a rapid recovery. The limitation of this study was the absence of histological confirmation of sarcoidosis.
Conclusion
Although cerebrovascular manifestation in sarcoidosis is uncommon, the clinical outcome can be quite serious if not treated rapidly and aggressively. Vasculitis manifestation of NS should be considered when recurrent infarcts and hemorrhage are encountered in the same patient, especially if clinical, radiological and biological signs of sarcoidosis are found and the differential diagnoses eliminated. More researches are needed to elucidate the real relationship between sarcoidosis and Moya Moya vasculopathy.
Declaration
Funding info: There are no funders to report for this submission.
Conflicts of interest: None declared under financial, general and institutional competing interests.
Ethics approval: The authors attest that the ethical consent for publication of this article was obtained from the patient.
Consent to participate: The authors give consent to participate in the preparation and the submission of this manuscript.
Written Consent for publication: The authors declare that they obtained written consent from the patient and that take fully responsibility over decisions to submit the manuscript for publication.
Availability of data and material: The authors attest that they had full access to all case data, take fully responsibility for the accuracy of the data analysis, have authority over manuscript preparation and that all data used in this case are available.
Code availability: Not applicable.
Authors Contributions
Dr. Rania Zouari: was responsible for writing the manuscript, analysis and interpretation of data.
Dr. Mohamed Zakaria Saeid: supplied the acquisition of data and revised the manuscript critically for better grammar and spelling content.
Prof Samia Ben Sassi: revised the manuscript critically for important intellectual content and gave final approval of the version to be submitted.
Cite this article
Rania Z, Zakaria SM, Samia BS. Moya-moya like vasculopathy secondary to sarcoidosis: a rare case report of concomitant ischemic infarcts and sub-arachnoid hemorrhage. Ann Neur Res Stud. 2023;2(1):1–6.