Cardiac Tamponade as the First Sign of Malignancy: A Case Report
* Sawana GS;
Gunaratnam M;
DiCicco E;
Aune J;
Mandava S;
-
* Sawana GS: Department of Medicine, University of Medicine and Health Sciences, Saint Kitts and Nevis.
-
Gunaratnam M: Department of Internal Medicine, McLaren Port Huron, MI, USA.
-
DiCicco E: Department of Internal Medicine, McLaren Port Huron, MI, USA.
-
Aune J: Department of Internal Medicine, McLaren Port Huron, MI, USA.
-
Mandava S: Department of Internal Medicine, McLaren Port Huron, MI, USA.
-
Nov 21, 2023 |
-
Volume: 4 |
-
Issue: 1 |
-
Views: 5934 |
-
Downloads: 1836 |
Abstract
Cardiac tamponade occurs when fluid or blood accumulates in the pericardial space, often resulting in reduced cardiac output and hemodynamic compromise. Malignancy is an uncommon cause of pericardial effusion, and cardiac tamponade being the first indication of malignancy, either primary or metastatic, is rare. In this case study, we present the instance of a 56-year-old woman with no known medical history, whose first sign of underlying malignancy was acute cardiac tamponade, emphasizing the importance of considering the possibility of hidden malignancies in patients with pericardial effusion, even when other clinical manifestations are absent.
Abbreviations
EKG: Electrocardiography; GI: Gastro-intestinal; CT: Computed Tomography; RT-PCR: Reverse Transcriptase- Polymerase Chain Reaction; JVP: Jugular Venous Pressure; IV: Intravenous; EGD: Esophagogastroduodenoscopy
Introduction
Cardiac tamponade is a life-threatening condition that occurs when fluid or blood accumulates in the pericardial space, leading to decreased cardiac output and hemodynamic compromise [1]. The most common causes of tamponade are trauma, myocardial infarction, and pericarditis, but it can also be a complication of malignancy [9]. It is rare for a cardiac tamponade to be the initial clinical manifestation of an unknown tumor, either primary or metastatic [4]. In this case report, we describe the case of a 56-year-old woman with no previous medical history who presented with acute cardiac tamponade as the first sign of underlying malignancy. She required an emergent pericardial window with drainage of pericardial fluid. Further investigation revealed likely primary lung metastatic adenocarcinoma [2]. This case highlights the importance of considering the possibility of underlying malignancy in patients presenting with cardiac tamponade, even in the absence of other obvious signs or symptoms.
Case Presentation
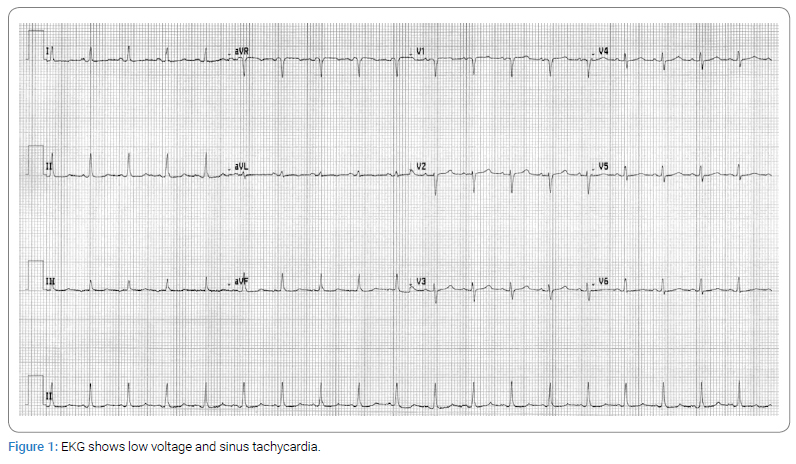
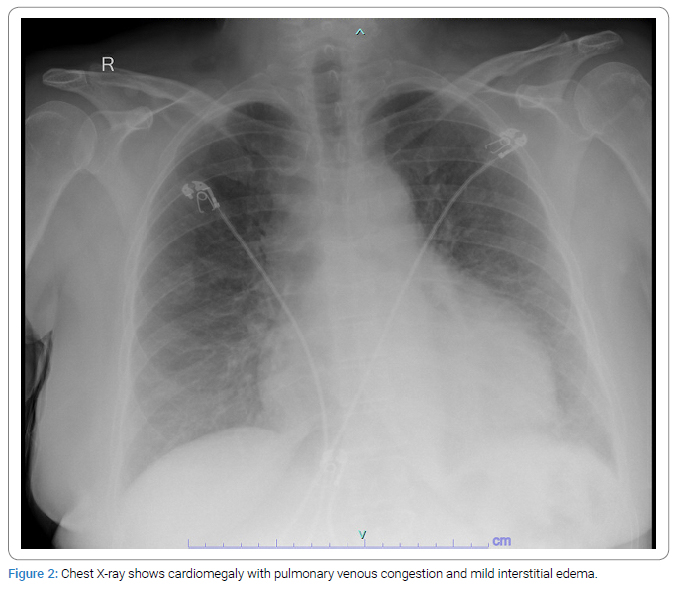
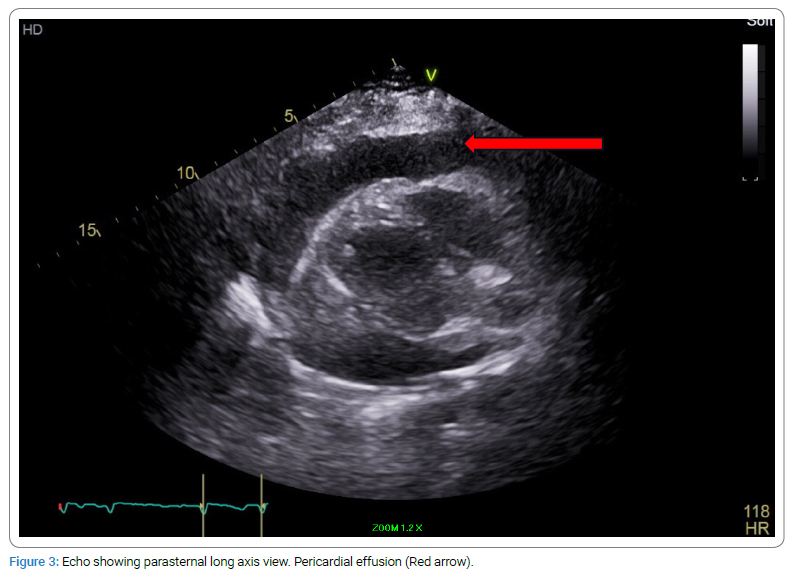
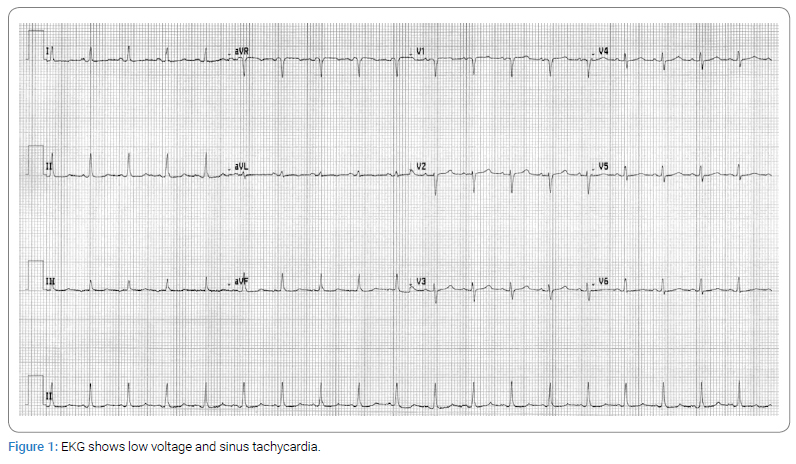
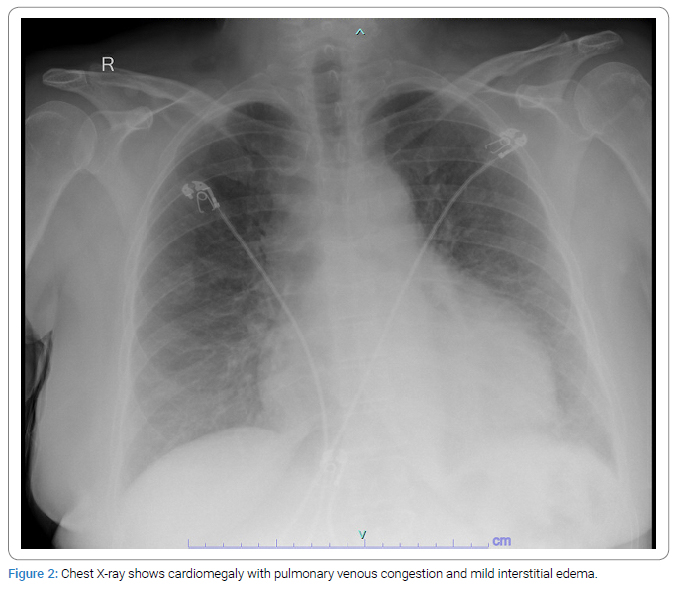
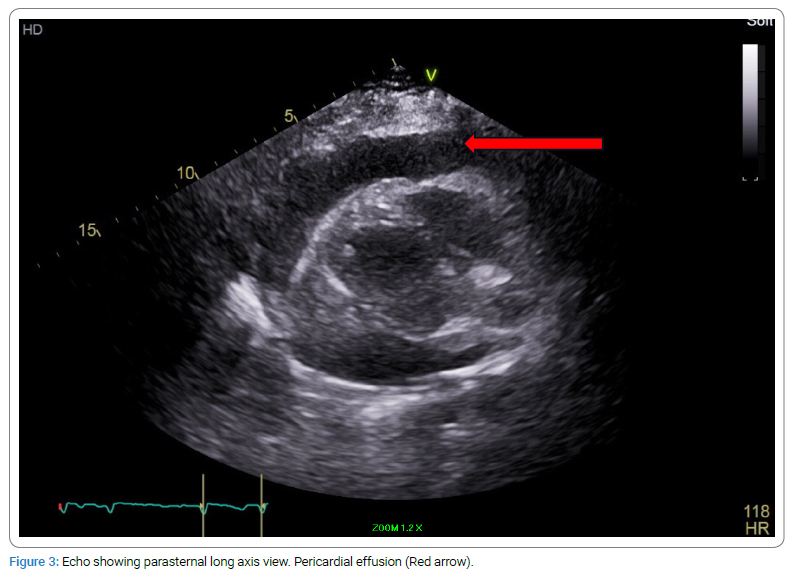
A 56-year-old woman with no significant past medical history presented to the emergency department with epigastric abdominal pain and shortness of breath. On arrival, her blood pressure was 86/65 mmHg, and her heart rate was 110 beats/minute. Her initial laboratory workup demonstrated neutrophilic predominant leukocytosis of 16.3 k/uL and creatinine of 1.34 with no baseline renal function available, likely representing acute renal failure. Electrocardiography (EKG) showed low voltage and sinus tachycardia (Figure 1). Chest X-ray showed cardiomegaly with pulmonary venous congestion and mild interstitial edema (Figure 2). Physical examination revealed elevated Jugular Venous Pressure (JVP) and distant heart sounds. A bedside 2-D echocardiogram (Figure 3) confirmed the suspicion of large pericardial effusion with tamponade physiology. The patient was immediately started on Intravenous (IV) fluids and required an emergent pericardial window with drainage of approximately 700 mL of sanguineous fluid. A pericardial fluid sample was sent for cytology review, and it was positive for metastatic adenocarcinoma. A pericardial tissue sample was sent for biopsy, and it was also positive for metastatic adenocarcinoma. The immunohistochemical analysis showed atypical cells positive for MOC 31 and CK7 but negative for Calretinin, CDX-2, CK20, Estrogen receptor, GATA3, Napsin A, PAX-8, and TTF-1 markers. The immunohistochemical marker pattern was nonspecific as to a potential primary site of origin. Differential diagnosis based on staining patterns included primary origin in the lung, breast, or upper GI/pancreaticobiliary tract, among other possibilities. Esophagogastroduodenoscopy (EGD) and colonoscopy with biopsy were also negative for any malignancy.
Further investigation revealed 2.7 cm x 2 cm right paratracheal soft tissue density on the Computed Tomography (CT) chest (Figure 4). Bronchoscopy was unsuccessful as the procedure was aborted early due to paroxysmal atrial fibrillation with rapid heart rate. Cancer Type ID, a Reverse Transcriptase- Polymerase Chain Reaction (RT-PCR) based assay, was utilized, which indicated lung cancer as the primary site with greater than 96% probability [11]. The patient received one-time doses of carboplatin and paclitaxel, with plans to get pembrolizumab. However, due to further decompensation of systolic heart failure, the patient was unable to tolerate further chemotherapy/immunotherapy and deceased within two months of initial presentation to the hospital.

Discussion
Pericardial effusion is the buildup of extra fluid in the space around the heart called pericardium [4]. A potential complication of pericardial effusion is cardiac tamponade [4]. Cardiac tamponade is a medical emergency that happens due to the accumulation of excess fluid in the pericardial sac, causing compression of the heart, leading to decreased cardiac output and shock [6]. There are a number of conditions that can cause pericardial effusion, such as malignancy, inflammation, injury, and idiopathic etiologies, but the leading cause is iatrogenic [7]. The most common malignancy that is associated with metastasis to the pericardium is lung cancer, followed by breast, hematological malignancies, and melanoma [4]. Malignant pericardial effusion is a slowly progressing clinically silent condition that rarely presents with hemodynamic instability and constitutes an initial manifestation of an underlying malignancy. Only 29% of the patients with metastases will have cardiac symptoms [10]. In most cases, cancer has been diagnosed based on clinical presentation other than the tamponade as a result of metastasis to the pericardium [3]. Malignant involvement of the pericardium has been identified in 5% to 20% of patients with metastatic neoplasms; however, the majority of studies show the incidence of cardiac tamponade manifesting as an initial presentation of an unknown underlying malignancy to be considerably low [5].
Therefore, cases like the one presented here are important for clinicians to keep a high index of suspicion for the possibility of cancer in patients presenting with tamponade, even in the absence of other obvious signs or symptoms [8]. Pericardiocentesis with analysis of the cytological fluid and additional immunohistochemical study, in some cases, is required for a definitive diagnosis [1]. Even though cytological fluid analysis is considered the gold standard of diagnosis and has lower false-negative rates than pericardial biopsy, negative cytology does not exclude malignancy in patients with a higher suspicion of secondary pericardial involvement [1]. Therefore, in such cases, a pericardial biopsy is required for further investigation [1]. Once the complications of neoplastic pericardial disease, such as cardiac tamponade, have been managed and diagnosis of neoplastic pericardial disease has been established, an individualized treatment plan for the patient should be established [3]. Early diagnosis and treatment of the underlying cancer may improve outcomes in these patients [3]. However, even with treatment of the underlying cancer, the prognosis is poor [3].
Conclusion
Cardiac tamponade as the first sign of malignancy is a rare but serious complication that can occur with any type of cancer. It is important for clinicians to consider the possibility of underlying malignancy in patients presenting with tamponade, even in the absence of other obvious signs or symptoms. Early diagnosis and treatment of the underlying cancer may improve outcomes in these patients.
Acknowledgments
Informed consent was obtained orally from the patient’s spouse before the documentation of this case report. We are unable to provide pathology images as pathology specimens were sent out to a different hospital for processing, and we were only able to access the pathology report.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003;349(7):684–690.
- Vemireddy LP, Jain N, Aqeel A, Jeelani HM, Shayuk M. Lung adenocarcinoma presenting as malignant pericardial effusion/tamponade. Cureus. 2021;13(3): e13762.
- Lewis MA, Hendrickson AW, Moynihan TJ. Oncologic emergencies: pathophysiology, presentation, diagnosis, and treatment. CA Cancer J Clin. 2011;61(5):287–314.
- Neves MBM, Stival MV, Neves YCS, da Silva JGP, Macedo DBR, Carnevalli BM, et al. Malignant pericardial effusion as a primary manifestation of metastatic colon cancer: a case report. J Med Case Reports. 2021;15(1):543.
- Almajed MR, Obri MS, Kamran W, Entz A. Malignant cardiac tamponade: a complication of untreated breast cancer. Cureus. 2022;14(7):e26787.
- Mehmood MA, Bapna M, Siddiqa A, Haider A, Saad M. Hemorrhagic pericardial effusion leading to cardiac tamponade: a rare initial presentation of adenocarcinoma of the lung. Cureus. 2020;12(11):e11411.
- Maisch B, Ristic A, Pankuweit S. Evaluation and management of pericardial effusion in patients with neoplastic disease. Prog Cardiovasc Dis. 2010;53(2):157–163.
- Li BT, Pearson A, Pavlakis N, Bell D, Lee A, Chan D, et al. Malignant cardiac tamponade from non-small cell lung cancer: case series from the era of molecular targeted therapy. J Clin Med. 2014;4(1):75–84.
- Babu RS, Lanjewar A, Jadhav U, Wagh P, Aurangabadkar G, Upadhyay P. A case series of malignant pericardial effusion. J Family Med Prim Care. 2022;11(10):6581–6585.
- Huntsman WT, Brown ML, Albala DM. Cardiac tamponade as an unusual presentation of lung cancer: case report and review of the literature. Clin Cardiol. 1991;14(6):529–532.
- Thomas SP, Jacobson LE, Victorio AR, Operaña TN, Schroeder BE, Schnabel CA, et al. Multi-institutional, prospective clinical utility study evaluating the impact of the 92-gene assay (Cancer TYPE ID) on final diagnosis and treatment planning in patients with metastatic cancer with an unknown or unclear diagnosis. JCO Precis Oncol. 2018;2:1–12.
Keywords
Pericarditis; Tumor; Adenocarcinoma; Tamponade
Cite this article
Sawana GS, Gunaratnam M, DiCicco E, Aune J, Mandava S. Cardiac tamponade as the first sign of malignancy: a case report. Clin Oncol J. 2023;4(1):1–4.
Copyright
© 2023 Sawana GS. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).