Pregnancy and Child Birth in Uterus Didelphys Associated With Ectopic Pregnancy and Longitudinal Vaginal Septum: A Case Report
* Brenda Nakitto;
Omondi E;
Okwonga A;
Ekak S;
Abel Odong;
-
* Brenda Nakitto: Faculty of Medicine, Gulu University, Gulu, Uganda.
-
Omondi E: Faculty of Medicine, Gulu University, Gulu, Uganda.
-
Okwonga A: Faculty of Medicine, Gulu University, Gulu, Uganda.
-
Ekak S: Faculty of Medicine, Gulu University, Gulu, Uganda.
-
Abel Odong: Department of Sexual Reproductive Health, Moyo General Hospital, Moyo, Uganda.
-
Dec 07, 2023 |
-
Volume: 2 |
-
Issue: 1 |
-
Views: 1868 |
-
Downloads: 922 |
Abstract
Background: Mullerian Duct Anomalies (MDAs) are congenital defects of the female genital system that arise from abnormal embryological development of the Mullerian ducts. This case report describes a rare case of a patient with uterus didelphys who successfully conceived, experienced an ectopic pregnancy in one uterus, and carried an intrauterine pregnancy to term in the other uterus, ultimately delivering via caesarian section.
Case: A 23-year-old G2P1+0 women from Abongi, Uganda, presented at 27 weeks gestation following the removal of a right-sided tubal ectopic pregnancy. At 13 weeks of gestation, a pelvic sonogram confirmed the diagnosis of a right-sided tubal ectopic pregnancy with no intrauterine pregnancy. At 39 weeks and 4 days gestation, the patient presented with labor-like pain. Despite no history of complicated prenatal care and no signs of preterm labor, the pregnancy in the left uterus progressed normally. The patient underwent a caesarian section due to a contracted pelvis and delivered a healthy child from the left uterus. Antibiotics were initiated post-delivery.
Conclusion: This case report highlights the successful management of a rare and complex reproductive scenario in a patient with uterus didelphys. It emphasizes the importance of early diagnosis through imaging modalities like trans-abdominal ultrasonography and MRI, comprehensive prenatal care, and individualized management strategies tailored to each patient’s specific circumstances.
Introduction
Mullerian Duct Anomalies (MDAs) encompass a spectrum of congenital defects affecting the female genital system, resulting from abnormal embryological development of the Mullerian ducts [1]. The embryological basis of MDAs involves the incomplete fusion, resorption, or development of the Mullerian ducts during fetal development [2]. Disruptions in the intricate processes of ductal development can lead to various anomalies and malformations of the uterus, fallopian tubes, and vagina [3], including uterine malformations such as uterus didelphys, uterus bicornis, septate uterus, and unicornuate uterus, among others [4]. The estimated incidence of MDAs in the general population ranges from 0.5% to 5.0%, with uterus didelphys representing a relatively rare subtype [5]. Uterus didelphys, is characterized by the presence of two separate uterine cavities with distinct cervices [6]. Patients often face reproductive challenges, including infertility, recurrent pregnancy loss, ectopic pregnancy, preterm labor, and malpresentation which are due to abnormal uterine structure, impaired uterine contractility, and altered endometrial receptivity [7].
While the classification and understanding of MDAs have advanced over the years, there is still much to learn about the optimal management and long-term outcomes for affected individuals. Each case presents a unique set of challenges, requiring individualized approaches to ensure the best possible reproductive outcomes for patients.
In this context, we present a case report of a patient with uterus didelphys who experienced both an ectopic pregnancy and an intrauterine pregnancy in separate uteri. The report highlights the complexities associated with MDAs, the successful management of the pregnancies, and the importance of comprehensive prenatal care in optimizing maternal and fetal outcomes.
Further research and evidence-based guidelines are needed to enhance our understanding of MDAs, improve diagnostic accuracy, refine treatment strategies, and provide appropriate counseling for affected individuals. By expanding our knowledge, we can better support patients with MDAs and offer them the best possible reproductive care.
Case Presentation
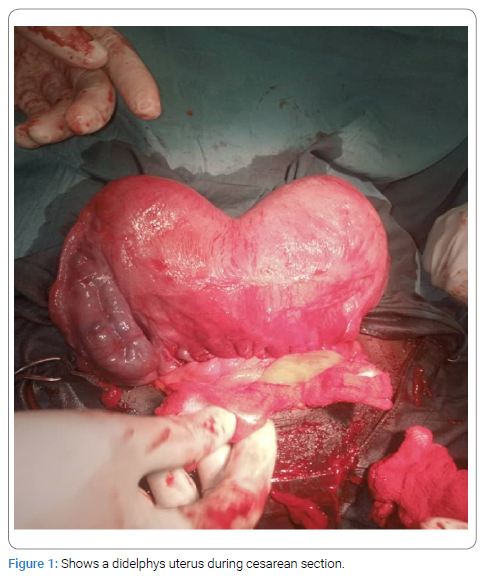
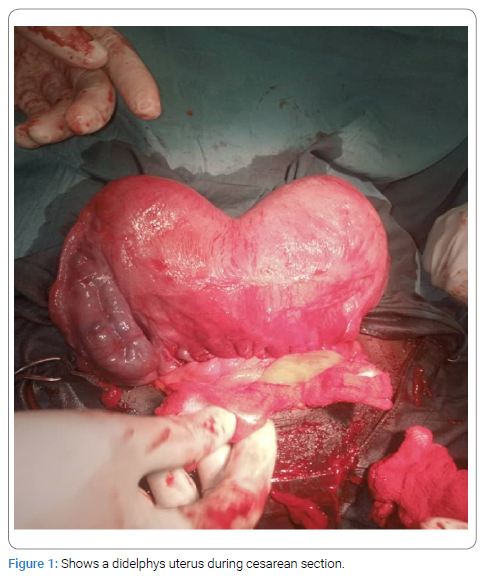
A 23-year-old unmarried female G2P1+0 At 39 weeks and 4 days of gestation was referred to the maternity unit of Moyo General Hospital from Luru Health Centre III with a 9-month history of amenorrhea and one day of lower abdominal pain. The patient experienced gradual, constant, moderate to severe pain radiating to the back, worsened by walking, not relieved by analgesics, accompanied by one day of clear watery non bloody fluid discharge. An emergency caesarian section was performed due to a contracted pelvis, revealing a gravid uterus on the left side and a non-gravid uterus on the right side (Figure 1). A live baby girl weighing 1900 gms with APGAR scores of 8 and 10 was delivered. The patient received postoperative care including antibiotics, analgesics, intravenous fluids, and wound dressing.
The patient had a previous cesarean section in 2019 due to a contracted pelvis, delivering a healthy baby boy, from a health center four to which the diagnosis of (MDA) was not documented. In November 2023, a pelvic sonogram confirmed the diagnosis of a right-sided tubal ectopic pregnancy at 13 weeks of gestation, however, this did not document the intrauterine pregnancy and the MDA, an exploratory laparotomy was performed extracting a right tubal ectopic pregnancy at 13 weeks of gestation with no documentation of the MDA.
Two weeks after the laparotomy, the patient reported abdominal movements to which the she thought to be a due to the laparotomy. In February 2024, an obstetric ultrasound was done following patients’ complaint of abdominal movements and enlargement, this confirmed an intrauterine pregnancy of 24 weeks gestation, the kidneys were of normal size, with no adnexal enlargement. The patient received appropriate antenatal care without any other reported maternal and fetal concerns during this pregnancy. The patient has a family history of normal vaginal deliveries, being the third born of 2 girls and 2 boys.
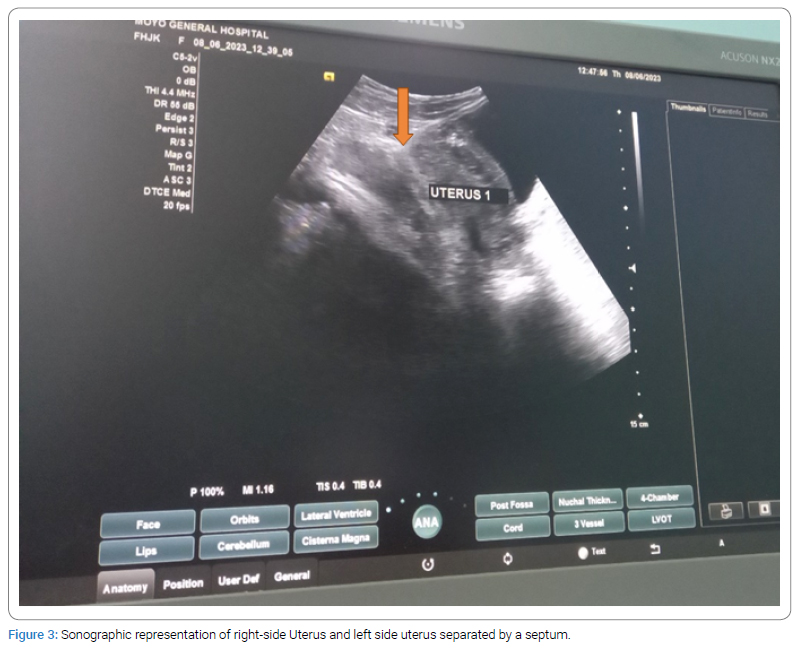
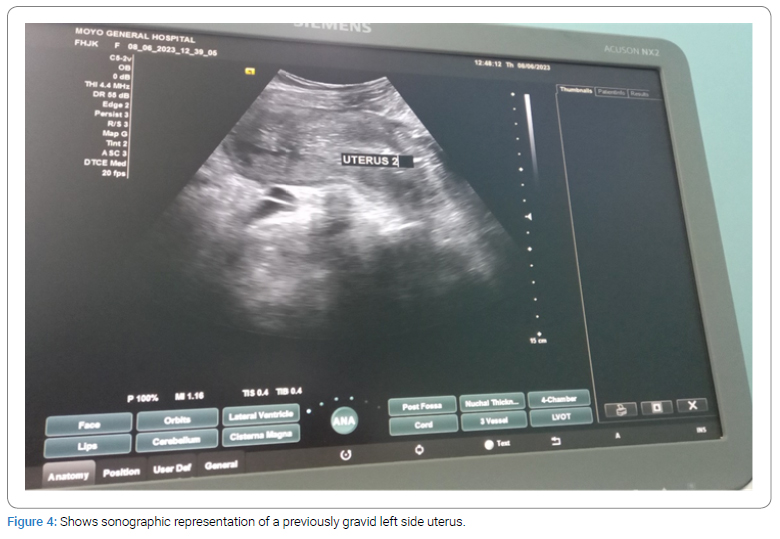
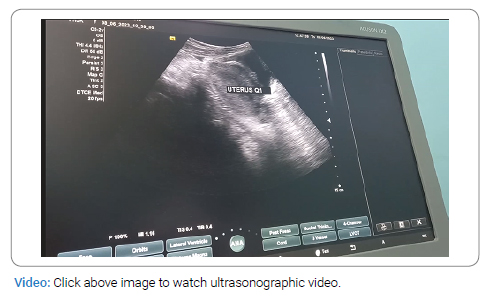
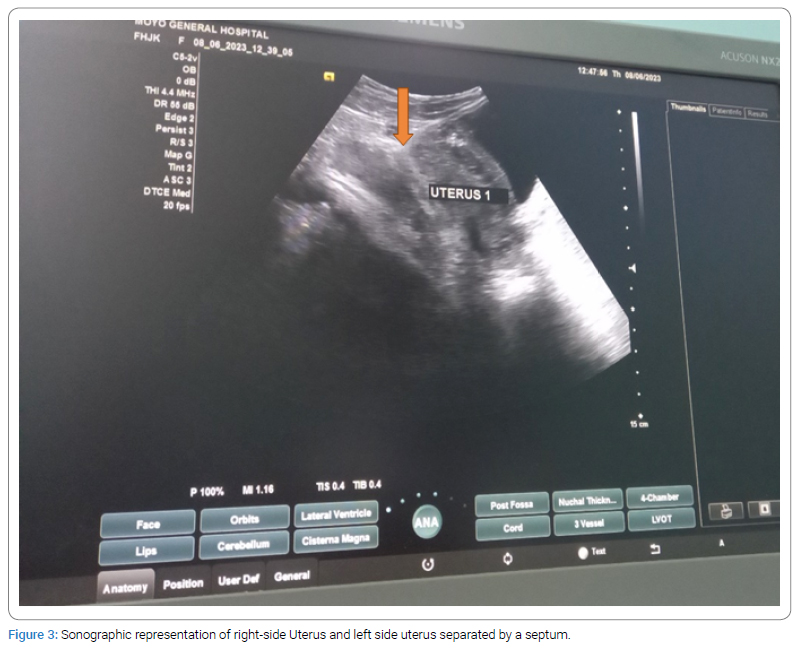
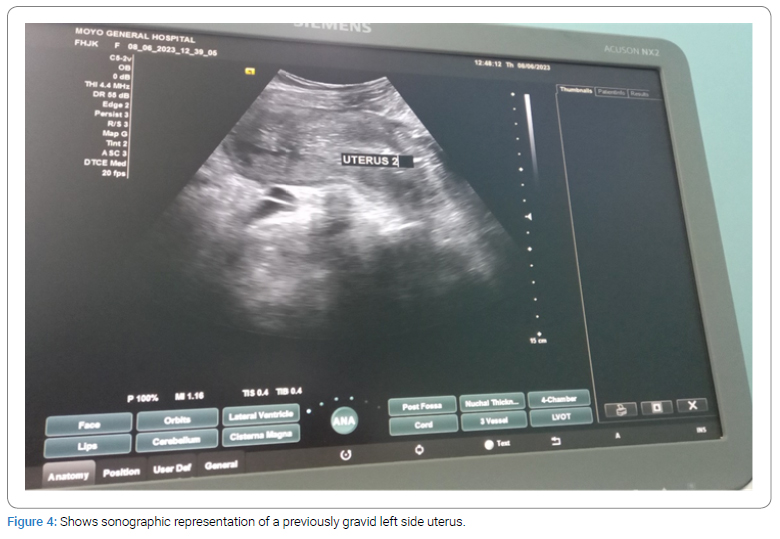
General physical examination revealed no obvious external abnormalities, and vital signs were within normal limits. The abdomen had a sub-umbilical midline incision, a well-contracted uterus with a fundal height of 14 cm. Vaginal examination revealed a longitudinal vaginal septum (Figure 2) with the urethra present and in its normal position. Trans-abdominal ultrasonography confirmed uterine didelphys with a single cervix (Figure 3 and Figure 4). The left uterus appeared larger than the right, the kidney was of normal size, ureters were present and well aligned, and other abdominal and pelvic organs were in normal size (Figure 4). However, MRI was not done since it’s not available in the rural setting.

The patient was discharged on the third post-operative day with oral antibiotics, analgesics, and open wound dressing. Stitch removal was scheduled for the seventh post-operative day.
Discussion
Uterus didelphys, a subtype of Mullerian Duct Anomalies (MDAs), is a rare congenital anomaly characterized by the presence of two separate uterine cavities with separate cervices [8]. The estimated incidence of MDAs in the general population ranges from 0.5% to 5.0% [7]. It is important to understand the clinical implications and challenges associated with uterus didelphys to provide appropriate management for affected individuals.
Diagnosis and Imaging Modalities
The diagnosis of uterine didelphys in this case was primarily confirmed through trans-abdominal ultrasonography, which is the mainstay imaging modality for diagnosing Mullerian duct anomalies (MDAs) [9]. This technique allows for the clear visualization of the distinct uterine cavities and helps in identifying additional anomalies, such as the longitudinal vaginal septum [10]. While Magnetic Resonance Imaging (MRI) can provide more detailed information about uterine anatomy, its availability in rural settings may be limited. Still, in more complex cases or for surgical planning, MRI can be a valuable tool to further evaluate the uterine structure [11].
Reproductive Challenges and Ectopic Pregnancy
The occurrence of an ectopic pregnancy in one uterus and an intrauterine pregnancy in the other uterus highlights the complex reproductive challenges in patients with uterus didelphys. Ectopic pregnancy is more common in patients with MDAs, with reported rates ranging from 11% to 40% [12]. The presence of two uteri with separate endometrial cavities and separate cervices increases the risk of implantation in abnormal locations, such as the fallopian tubes [13].
Prompt diagnosis and management of ectopic pregnancies are crucial to prevent complications and preserve fertility.
Antenatal Care and Pregnancy Management
The successful progression of the intrauterine pregnancy in the left uterus in this case demonstrates the potential for a favorable outcome in patients with uterus didelphys. However, close monitoring and individualized antenatal care are essential to identify any potential complications, such as preterm labor or cervical incompetence [14]. Regular ultrasound examinations, assessment of cervical length, and fetal well-being monitoring are important components of prenatal care in these patients [14].
Mode of Delivery Considerations
The decision to perform a caesarian section in this case was based on the contracted pelvis, which is a known complication associated with uterus didelphys. However, the mode of delivery should be determined on a case-by-case basis, considering factors such as the maternal and fetal conditions, pelvic anatomy, and the experience of the healthcare team. Vaginal delivery may be feasible in selected cases, particularly when the pelvic dimensions allow for safe passage of the fetus.
Conclusion
In conclusion, this case report highlights the successful management of a rare and complex reproductive scenario in a patient with uterus didelphys. It emphasizes the importance of early diagnosis through imaging modalities like trans-abdominal ultrasonography and MRI, comprehensive prenatal care, and individualized management strategies tailored to each patient’s specific circumstances. These diagnostic tools aid in the selection of the most suitable treatment strategies, including surgical interventions, reproductive techniques, and obstetric management. Accurate diagnosis of MDAs is crucial for appropriate management and counselling. Further research and case reports are warranted to enhance our understanding of the clinical outcomes and optimal management approaches for patients with uterus didelphys.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Informed consent was obtained for this publication.
References
- Olpin JD, Moeni A, Willmore RJ, Heilbrun ME. MR imaging of Müllerian fusion anomalies. Magn Reson Imaging Clin. 2017;25(3):563–575.
- Sugi MD, Penna R, Jha P, Pōder L, Behr SC, Courtier J, et al. Müllerian duct anomalies: role in fertility and pregnancy. Radiographics. 2021;41(6):1857–1875.
- Pitot MA, Bookwalter CA, Dudiak KM. Müllerian duct anomalies coincident with endometriosis: a review. Abdom Radiol. 2020;45(6):1723–1740.
- Yoo RE, Cho JY, Kim SY, Kim SH. A systematic approach to the magnetic resonance imaging-based differential diagnosis of congenital Müllerian duct anomalies and their mimics. Abdom Imaging. 2015;40(1):192–206.
- Al-Basri SF, Raheem EAA, Agamy A, Qaria R, Al Hachim EG, Shamrani H, et al. Uterus Didelphys with Obstructed Hemivagina: A Report of Three Cases. J Clin Case Stu. 2017;2(4).
- Leanza V, Incognito GG, Gulisano M, Incognito D, Correnti SG, Palumbo M. Herlyn-Werner-Wunderlich syndrome and central placenta previa in a COVID-19 positive pregnant woman: A case report. Ital J Gynaecol Obstet. 2023;35(2):136–141.
- Grimbizis GF, Camus M, Tarlatzis BC, Bontis JN, Devroey P. Clinical implications of uterine malformations and hysteroscopic treatment results. Hum Reprod Update. 2001;7(2):161–74.
- Heinonen PK. Uterus didelphys: a report of 26 cases. Eur J Obstet Gynecol Reprod Biol. 1984;17(5):345–350.
- Acién P, Acién M, Sánchez-Ferrer ML. Müllerian anomalies “without a classification”: from the didelphys-unicollis uterus to the bicervical uterus with or without septate vagina. Fertil Steril. 2009;91(6):2369–2375.
- Banks E, Beral V, Bull D. Bibliography current world literature vol 15 no 6 december 2003. Pharmacogenomics. 2003;4:269–277.
- Li Y, Phelps A, Zapala MA, MacKenzie JD, MacKenzie TC, Courtier J. Magnetic resonance imaging of Müllerian duct anomalies in children. Pediatr Radiol. 2016;46(6):796–805.
- Troiano RN, McCarthy SM. Mullerian duct anomalies: imaging and clinical issues. Radiology. 2004;233(1):19–34.
- Fylstra DL. Ectopic pregnancy not within the (distal) fallopian tube: etiology, diagnosis, and treatment. Am J Obstet Gynecol. 2012;206(4):289–299.
- Hiersch L, Attali E, Melamed N. Special considerations regarding antenatal care and pregnancy complications in dichorionic twin pregnancies. Am J Obstet Gynecol MFM. 2022;4(2S):100500.
Keywords
Ectopic pregnancy; Mullerian duct anomalies; Uterus didelphys
Cite this article
Nakitto B, Omondi E, Okwonga A, Ekak S, Abel Odong. Pregnancy and child birth in uterus didelphys associated with ectopic pregnancy and longitudinal vaginal septum: a case report. Glob J Gynecol Obstet Res. 2023;2(1):1–5.
Copyright
© 2023 Brenda Nakitto. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).