Abstract
Tuberculosis is an infectious disease which still remains a public health problem, especially in the Third World. The delay in its diagnosis determines contributes to the spread of the disease. The objective of this present study was to describe the epidemiological and clinical aspects of tuberculosis and to search for factors related to diagnostic delays. This is a prospective, descriptive and analytical study of patients seen in the pneumology department of the Tambohobe University Hospital Center in Fianarantsoa (CHUT) Madagascar from July 1 to December 15, 2018. The average age was 37.01 years with a range from 16 years to 86 years. The female gender represented 53.90% (n = 102) with a sex ratio of 0.85. The history of patients found was dominated by chronic alcoholism in 48.03% (n = 102) and smoking in 45.09% of cases. The average diagnostic delay in our study was 115.97 days. The delay of the healthcare system was 57.66 days. The patient delay was long (63.4 days). A history of chronic alcoholism is a diagnostic delay factor related to the healthcare system (0R = 2.427). In our study, the presence of diarrhea (0R = 10.440) was a factor in delaying the diagnosis of tuberculosis, while dyspnea contributes to shortening the time to diagnosis (0R = 0.35 95% CI) [0.141–0.875].
Knowing these factors helps to control the progression of this disease. Continuing medical training for health personnel and awareness of the population an asset to limit this diagnostic delay.
Introduction
Tuberculosis is an old but still relevant disease. It is an infectious, contagious disease, mainly transmitted between humans by air and mainly due to Koch's bacillus or Mycobacterium tuberculosis. Today, treatments make it possible to properly care for people with this disease, which can be prevented by vaccination. However, tuberculosis remains one of the top 10 causes of morbidity and mortality in the world. Caregivers, researchers and governments are on the front line in the fight against this pathology, which despite everything remains a major public health issue, in Madagascar as elsewhere in the world. The World Health Organization (WHO) identified 10 million new cases of tuberculosis worldwide in 2018. The majority of these people were between 15 years and 50 years old. The disease thus affects millions of working people around the world, which is not without economic and social consequences in the countries concerned [1].
In Madagascar, tuberculosis remains endemic. According to WHO statistics in 2015, the prevalence of tuberculosis on the Big Island is around 413 cases per 100,000 inhabitants. The UN body also estimates that 12,500 people died of the disease that year: an incidence of 52 deaths per 100,000 inhabitants and support the epidemic. Delays in the diagnosis of tuberculosis contribute to the spread of the disease. Early diagnosis of tuberculosis and effective and rapid treatment are necessary to best control the disease. The population must also be made more aware of the benefits of being vaccinated [2]. To better understand, we conducted a survey within the pneumology department of the University Hospital Center (CHU) of Tambohobe in Fianarantsoa, which aims to describe the epidemioclinical aspects of tuberculosis and to seek factors related to diagnostic delays.
Methodology
Our study took place in the Pneumology department of the Tambohobe University Hospital Center in Fianarantsoa (CHUT). The CHUT is located in the Haute Matsiatra region, province of Fianarantsoa, Madagascar. This is a prospective, descriptive and analytical study of patients seen in the pneumology department, in whom tuberculosis was newly diagnosed, from July 01, 2018 to December 15, 2018. The study population was patients hospitalized for tuberculosis, whatever the location or form of the disease. All patients newly diagnosed with tuberculosis, all forms combined and over the age of fifteen were included in the study. The data was collected from a standard questionnaire, questioning the patients as soon as their diagnosis was established. We used Microsoft Office Word and Excel 2010 software and SPSS Statistics 22 software for data processing and analysis, calculations and statistical tests of the results. The Chi-square test was used to verify the existence of an association. It was significant if p is less than 0.05. The logistic regression test was used to obtain the Odds Ratio (OR). The variables studied were the epidemiological parameters, the distances between the health center and the patient's home, the modes of transport, the history, the clinical parameters, the paraclinical data, the diagnostic delay, the therapeutic parameters: the status and the number of doctors consulted before the diagnosis; the type of hospitalization.
The variables studied
a) Epidemiological parameters: age; gender; occupation; address; level of instruction;
b) Distances between the health center and the patient’s home
c) Modes of travel
d) Background
e) Clinical parameters: general signs; functional signs; the signs physical
f) Paraclinical data (radiography and biology)
g) Diagnostic delay
h) Therapeutic parameters: the status and number of doctors consulted before the diagnostic; the mode of hospitalization
During our study, the following diagnostic delays were defined:
- Patient delay: this is the time that elapses between the onset of symptoms and the first consultation with a practitioner. It is considered long when it exceeds thirty days.
- Healthcare system delay: this is the delay between the first consultation with a healthcare professional and the start of treatment. It is considered long when it exceeds thirty days.
- Total time: this is the time that elapses between the appearances of the first signs until the start of treatment. The total delay is considered long when it exceeds sixty days.
The level of education was classified as follows:
- Primary: 12th grade to 7th grade;
- Secondary level I: 6th grade to 3rd grade;
- Secondary level II: second class up to terminal class;
- University: all studies carried out after the Baccalaureate.
We considered that patients knew the symptoms of tuberculosis when they responded with a “chronic cough”.
We considered that the patients knew the mode of contamination of tuberculosis when they answered by “cough”.
We asked patients to estimate the number of weeks between the onset of symptoms and seeking medical care.
Symptoms most commonly associated with TB are classified as TB, and include anorexia, chest pain, chills, cough, fatigue, fever, hemoptysis, night sweats, and weight loss.
All other symptoms less frequently associated with TB were classified as non-TB.
Results
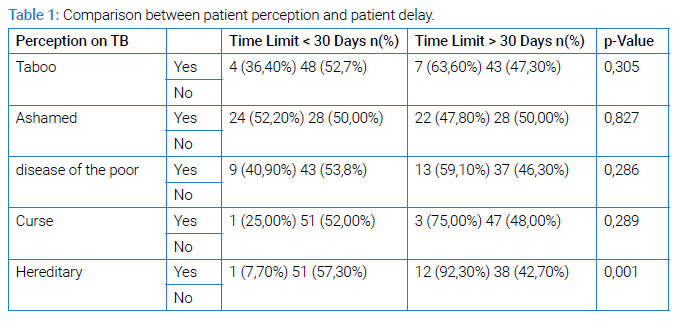
During the study period, 328 patients were admitted to the pulmonology department for medical pathologies, of which 217 were diagnosed with tuberculosis. 200 questionnaires had been shared among the patients. 102 people agreed to answer, a participation rate of 51%. During this study, 71 people had pulmonary tuberculosis, i.e., 70% of the patients; 31 patients were followed for extra-pulmonary tuberculosis, all forms combined, i.e., 30% of the people hospitalized (n = 102). The average age was 37.01 years with a range of 16 years to 86 years. The female gender represented 53.90% (n = 102) with a sex ratio of 0.85. Category 2 occupation represented 61.80% of patients (n = 102). The majority of our patients were in the primary level at 44.10% (n = 102). The population residing in the urban area constituted 62.70% (n = 102) of the cases. In our study, 61.76% (n = 102) of the patients were married and 45.10% of the patients believed that tuberculosis is a shameful disease. Seventy-four point five percent of our patients knew their treatment was free. The history of patients found was dominated by chronic alcoholism in 48.03% (n = 102) and smoking in 45.09% of cases. For their first consultation, 51.96% (n = 102) of patients went to a general practitioner at the public hospital. The search for AFB in the sputum was the assessment prescribed in the first consultation in 32 cases, or 31.37% (n = 102) of the examinations carried out. All of the delays we looked at were long: patient delay, healthcare system delay, and total delay. None of the demographic parameters were associated with time to diagnosis. The belief that tuberculosis is hereditary was significantly related to patient delay with p = 0.001 (Table 1).
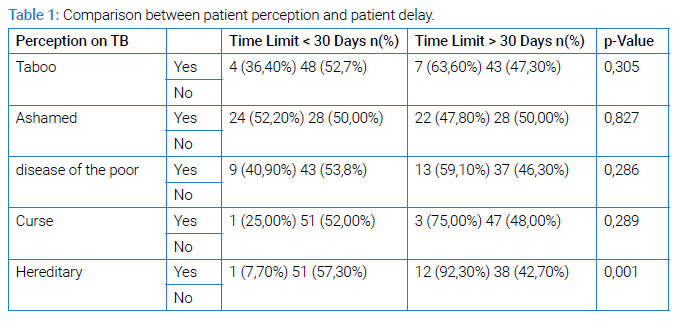
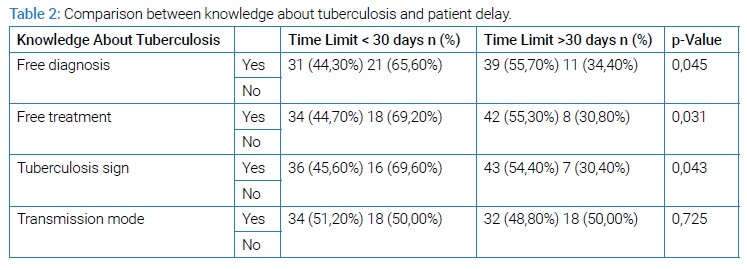
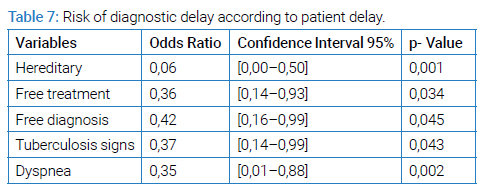
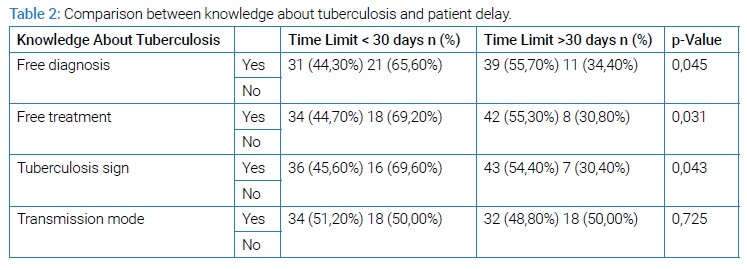
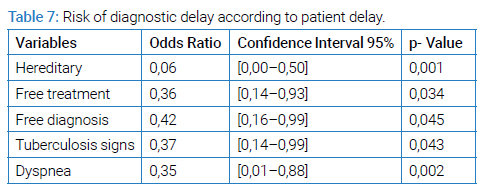
Regarding the relationship between knowledge about tuberculosis and patient delay, knowing the free treatment and diagnosis and the signs of tuberculosis was significantly positively associated with patient delay (Table 2).
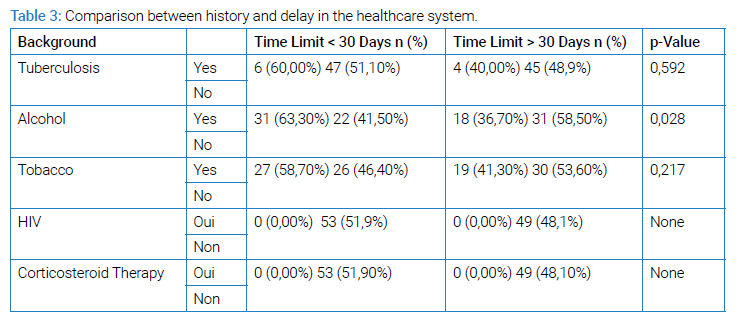
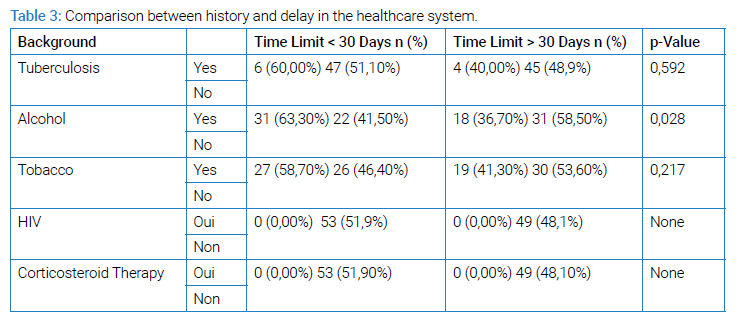
Patient history had no relationship with total diagnostic delay.
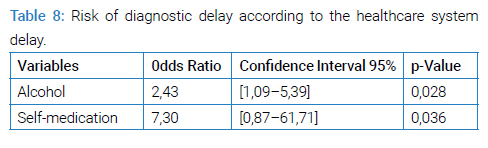
Chronic alcoholism was significantly linked to longer delays in the healthcare system (p = 0.028) (Table 3).
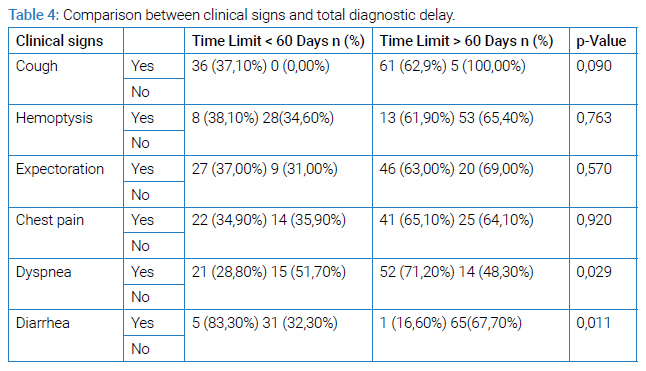
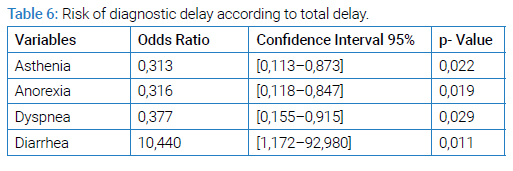
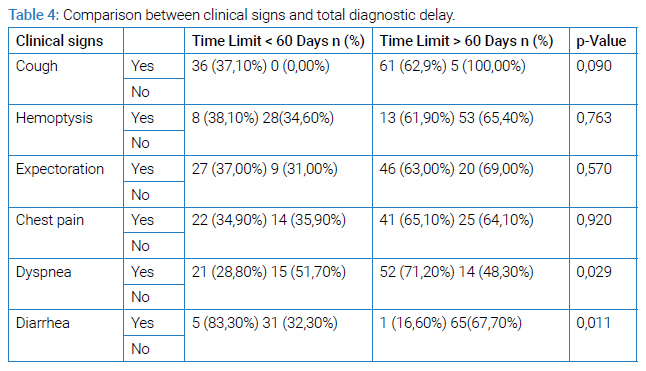
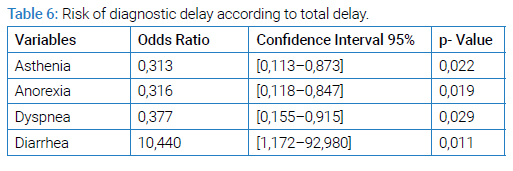
The presence of dyspnoea and diarrhea was significantly related to the longer total diagnosis delay p = 0.029 and p = 0.011 (Table 4).
The clinical signs were not associated with the delay in the healthcare system. The choice of first consultation made by the patients was not associated with the total diagnosis delay.
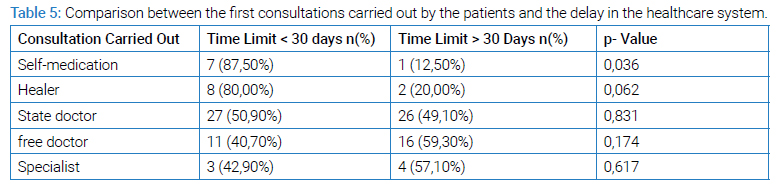
The patient delay did not depend on the first consultations made by the patients.
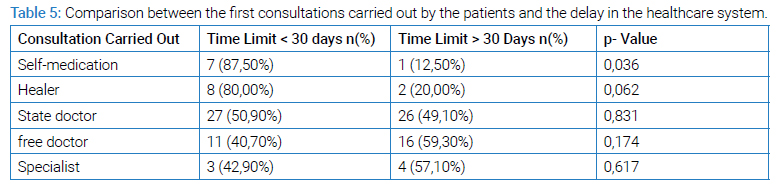
The fact of self-medication was significantly related to the longest delay in the care system p = 0.036 (Table 5).
The radiological signs had no relationship with the delay of the healthcare system.
The presence of diarrhea was a delay factor in establishing the diagnosis. The following elements were a factor shortening the total time to diagnosis of tuberculosis: the presence of asthenia p = 0.022, anorexia p = 0.019 and dyspnoea p = 0.029 (Table 6).
According to patient delay, the presence of dyspnea, patient knowledge of the signs, free diagnosis and treatment and belief in tuberculosis were all factors shortening patient delay (Table 7). According to the care system delay, self-medication and chronic alcoholism were factors in the delay of diagnosis for the staff.
Discussion
In our study, the average age of the patients was 37.01 years, the youngest being 16 years old and the oldest 86. During our investigation, we did not find a link between age and the delay in diagnosis. Comparable to the study carried out in Madagascar, Nigeria and Tanzania [3–5]. However, there are other studies that claim the opposite. This is particularly the case of the surveys carried out in Cameroon in 2012 [6], in Asia [7], in Angola [8], in the North-West of Ethiopia [9], in the Center-North of Ethiopia, in the town of Dessie [10].
During our study, we were able to observe a female predominance among the patients, with a sex ratio of 0.85 similar to a study carried out at the Jamot hospital in Yaoundé [11]. There is no data that allows us to statistically associate gender with the types of delay in diagnosis of tuberculosis. Our survey also shows that the factors favoring tuberculosis can be found with equal frequency in both sexes, as well as risk factors such as alcohol or tobacco. Madagascar is still a country with a high endemicity of tuberculosis despite the establishment of the National Tuberculosis Control Program (NTCP) since 1991 [12]. The interest of our study is based on the consistency of the data collected with the conclusions of other surveys carried out elsewhere in the world. Thus, our study joins that which was carried out in Algeria [13] in 2016, in Tanzania [5] in 2016 and in North-Central Ethiopia [10] in 2017 showed similar results, concluding, like the one we conducted, that the gender is not one of the diagnostic delay factors. This does not prevent there from being discrepancies between studies that are equal. Thus, contrary to what we have seen, studies conducted in countries with limited resources [14] such as Bangladesh [11] or Peru [15] support the existence of a link between gender and delayed diagnosis.
No data allows us to establish a link between the level of study of the patients and the time that elapses between the appearance of the first symptoms and the consultation of a doctor then the management by a health center. Another study, conducted at the USFR de Pneumologie de Befelatanana, goes in the same direction [3]. However, the scientific literature includes studies that claim the opposite [16–18]. These indeed underline that for patients with a primary level of education, the time to diagnosis is longer compared to those with a higher level of education. This can be explained by people with a low level of education who are mostly unfamiliar with tuberculosis. Some of them do not always have the reflex to consult a doctor even when the first clinical signs appear. The link between low level of education and delayed diagnosis can also be explained by the patients in question most often living in precarious conditions. If some do not go to the doctor because they are unaware of the disease, others do not go because they cannot afford it [19,20]. Two African studies [17,21] also show that poorly educated patients are diagnosed twice as long as the others after the appearance of the first symptoms.
Some patients were convinced that tuberculosis is a hereditary disease. During our study, we were able to observe that this belief is one of the factors that can lengthen the patient delay. In Manila, Portero et al., [22] reported that nearly a third of respondents thought TB was an inherited condition. Watkins and Plants [23] have also reported that many Balinese share this belief, with some even associating the disease with magic or an environment deemed unclean.
Our survey reveals that patient knowledge of the signs (chronic cough) and free diagnosis and treatment was a factor shortening patient delay (Table 7). In 2016, in Georgia [24], M. Djibuti concluded in the same way (OR at 0.35; 95% CI [0.12–0.99]. Four other studies support that when patients are unfamiliar with the disease, they take longer to see a doctor. The studies in question have been carried out in China [25], Ethiopia [26], Mozambique [27] and Malawi [2]. Lack of knowledge of the disease is not, however, the only factor that can delay the diagnosis of tuberculosis. Indeed, it also happens that patients who know the disease well (its signs, its modes of transmission, etc.) are diagnosed late OR = 0.24, p = 0.031) [29]. If these people take time to consult a doctor, it is sometimes also because they believe that tuberculosis is a shameful disease.
The average diagnostic delay in our study was 115.97 days (four months). In Ethiopia, a study highlighted that the average duration between the onset of symptoms and the first consultation was 5.9 months [30]. This particularly long delay not only leads to severe forms of the disease but promotes the contamination of more people in the community. Some countries where tuberculosis is highly endemic also record significant delays in diagnosis. This is the case, for example, of Tanzania where the diagnostic delay can reach 136 days [31], Mozambique (150 days) [27] and Ghana (120 days) [32].
Some industrialized countries are not spared, such as the United Kingdom (78 days) [33], the United States (89 days) [34] and East London (126 days) [35]. In our study, the patient delay was long (63.4 days). It is comparable to the delays observed during studies carried out in Ethiopia (60 days) [30] or in Tanzania (120 days) [31]. These delays are in stark contrast to what we see in other countries. For example, a particularly short patient delay was observed in southern India: 20 days [36]. The patient delay is an important indicator that allows getting an idea of the knowledge of tuberculosis patients. The delay is long when the population studied is not very sensitized or knows little about the origins or the symptoms of the disease.
With regard to the delay of the healthcare system, that which elapses between the first consultation and the start of treatment, we noted, during our investigation, a delay of 57.66 days. This delay is comparable to those observed in Georgia in 2013 by AS Rabin (56.2 days) [37] and in Malawi in 2014 (59 days) [28]. However, some countries record much longer delays, in particular Uganda [38] and Uzbekistan [39]: 77 days and 128 days respectively. In Zimbabwe, on the other hand, a much shorter delay was observed: 2 days [40]. These differences could be explained by the different countries not using the same criteria to define the delay of the healthcare system. Added to this is the lack of experience of some health professionals in the management of tuberculosis or the lack of resources of the health services [41].
During our study, we found that 7.84% of patients had already experienced self-medication before consulting a health professional. However, this reflex is one of the factors delaying the delay of the healthcare system. Seid A et al, in his study carried out in 2017 in North-Central Ethiopia [10], found that the practice of self-medication was among the main factors prolonging the patient's delay (AOR = 3.0 CI 95 %: [1.3–5.6]): clearly, the people thus studied take longer to consult a health professional when the first symptoms appear. In 2015, in the Arsi area [42], Abdulbasit Hamza also reported that the practice of self-medication delayed the establishment of a diagnosis and therefore the management of patients (OR 10.82 95% CI 5.09 -22.98). Belkina TV et al., [39], in Uzbekistan in 2014, also reported that self-medication was the first reflex of many patients when faced with the appearance of symptoms of tuberculosis (p = 0.005). The role that self-medication plays in delaying the diagnosis and management of patients is also confirmed by various Ethiopian reports [43–45].
In our study, 48.03% of patients were alcoholic and 45.09% smoker. A history of chronic alcoholism is a diagnostic delay factor related to the healthcare system (0R = 2.43) (Table 8).
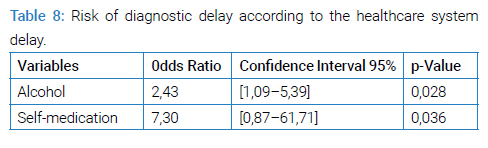
Drug addiction increases the risk of developing tuberculosis. In Tunisia, in 2014, J Ben Amar [46] showed that diagnostic times were longer in patients with alcohol dependence. In Arsi, in 2015 [42] and in Portugal [47], studies came to the same conclusion. Another study, carried out in Tanzania [31], had also established a link between the consumption of substances such as alcohol and tobacco and the delay in patient care. Other studies, carried out in Angola [48] and India [36], come to the same conclusion. Two other studies, conducted in China in 2011 [49] and at the Befelatanana USFR de Pneumologie in 2015 [3] also confirm the causal link between smoking and increased patient delay.
In our study, the presence of diarrhea (0R = 10.440) (Table 6) was a factor in delaying the diagnosis of tuberculosis, while dyspnea contributes to shortening the time to diagnosis (0R = 0.35 95% CI) [0.141–0.875]. The result of our investigation is similar to the conclusion of a study conducted in 2015 by Ravahatra K in the pneumology department of Befelatanana (OR: 0.3556, IC: [0.1283–0.9852]) [3]. Asthenia and anorexia with ratio odds of 0.316 and 0.313 respectively (Table 6) are factors that shorten the total time taken to treat patients, as we observed during our study. On the other hand, Ravahatra K concluded in 2015 [3] that the presence of asthenia (OR = 2.952) and anorexia (5.4815) rather tends to delay the diagnosis of tuberculosis. The same study supports that the delay of the healthcare system is shorter with asthenia with an odds ratio of 0.1081. Two studies [50,51] also support that the general signs can lead to a delay in the diagnosis of tuberculosis.
In our study, only 31.37% of patients had undergone sputum examinations and 23.53% chest X-rays during their first visit to a health professional. A New Zealand study reported that in many cases, the first doctor seen by the patient did not perform an x-ray, ask about tuberculosis or obtain a sputum smear and this even if the subject had classic symptoms [52]. The same observations were made by Ward et al in Australia [53]. A study, carried out in Switzerland, had shown that having undergone a chest X-ray during the first consultation could reduce the delay of the healthcare system [54]. Another study, carried out in northern Ethiopia [10], underlines that the diagnosis of tuberculosis using a chest X-ray 0R = 0.32 considerably reduces the delay of the health system compared to microscopy. This finding is consistent with reports by Chen et al., [55] in Taiwan, which indicate that for 17% of patients diagnosed on the basis of symptoms and chest X-ray, no health system delay was found.
During our study, we note that only 24 (23.53%) doctors prescribed a chest X-ray and only 32 (31.37%) prescribed the search for AFB in the sputum, in the presence of clinical signs related to tuberculosis. Studies carried out in other countries have similarly reported an underuse of sputum examinations by private physicians [28,56]. A normal x-ray and negative smear results were among the delay factors of the healthcare system [57]. This reality is valid in Madagascar as elsewhere in the world [40,58]. During our study, sputum microscopy was the main method of investigation when a subject was suspected of having tuberculosis, as the GeneXpert method had not yet been tested in the country. Our study has its limits. Given that this is a prospective study, certain estimates (those relating to delays in diagnosis or management) are imprecise, in particular due to the memorization bias in patients.
The fact that the patients do not clearly remember when the first symptoms appeared or on which date they decided to consult a health professional may have influenced the data we collected. In addition, the sample sizes are tiny, which limits the possibility of performing further statistical analyzes on factors associated with delays in diagnosis or treatment. The survey was conducted in a single hospital establishment, the CHU of Fianarantsoa, which does not allow us to generalize the conclusions drawn from the data collected. It is possible that different or at least more nuanced realities can be observed in other health centers or in private establishments.
Conclusion
Tuberculosis is still an endemic disease in Madagascar. The precariousness of patients is one of the main factors delaying diagnosis. The lack of financial means dissuades many families from going to consult health professionals when the first signs appear, especially when these are too general to evoke tuberculosis, such as cough, fever or night sweat. The average delay of patients that of the healthcare system and the total delay were respectively 63.4 days, 57.66 days and 115.97 days. The healthcare system itself also reacts late in some cases, sometimes due to ignorance of the symptoms or lack of resources. Alcohol history and self-medication are among the factors delaying diagnosis, which can also have repercussions on the responsiveness of the healthcare system. The same is true for the presence of diarrhea, asthenia, anorexia or even dyspnea.
Cite this article
Razafimpihanina SM, Rasoafaranirina MO, Razafindrasoa AZ, Ramandray F, Andriarimanga DO, Rakotondranaivo AW, et al. Epidemioclinical profile and factors associated with delayed diagnosis of tuberculosis seen at the chu of fianarantsoa in madagascar. 2023;1(2):1–8.