Abstract
Methemoglobinemia is one of the rare but fatal causes of cyanosis in which hemoglobin gets oxidized changing its Ferrous (Fe2+) state to a ferric state (Fe3+) and so methemoglobin is unable to bind oxygen and deliver it to tissues despite the adequate concentration of oxygen in the blood. Causes can be congenital or acquired; the acquired causes include exposure to different chemicals like benzocaine, dapsone, herbicides, pesticides, nitrobenzene, aniline, and fumes from combustion engines. Dapsone-induced methemoglobinemia has been reported often in case reports and research studies along with concurrent anemia and pneumonia, at high doses (more than the target dose of 2 mg/kg/day) or taken for long duration in the majority of case reports. Here is a case of dapsone-induced methemoglobinemia in a middle-aged lady at a very low dose taken for a very short period, keep in mind that dapsone-induced methemoglobinemia even at a low dose for a short period. Methemoglobin levels in the blood cannot be checked in Pakistan due to the unavailability of pertinent tests. Methemoglobinemia is a fatal disorder affecting the carrying capacity of blood. The methemoglobin reduction system is responsible for keeping haem in reduced form, the form that is responsible for carrying oxygen. When this balance of oxidation and reduction is disturbed by oxidants, an abnormal form of hemoglobin is formed i.e. methemoglobinemia occurs [1].
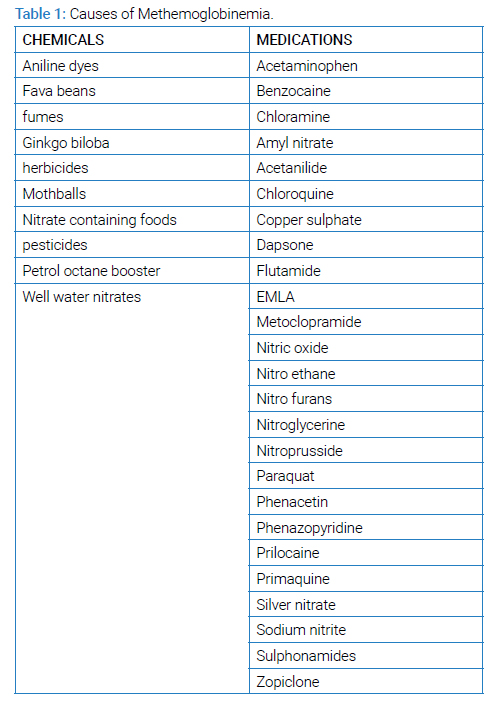
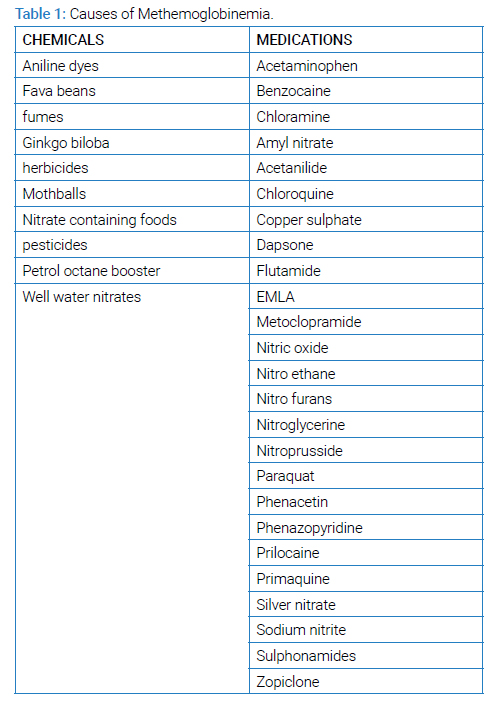
The two main mechanisms that keep methemoglobin levels less than 1% are the cytochrome b5-MetHb reductase pathway and the pathway involving nicotinamide adenine dinucleotide phosphate (NADPH)-MetHb reductase. Causes of MetHb can be genetic or acquired. Genetic causes are deficiency of cytochrome b5 reductase pathways. Acquired causes can be due to exposure to different chemicals like Toxins and environmental contaminants, most notably nitrates, chlorates, aniline compounds, dapsone, and benzocaine [2], (Table 1). Long-term dapsone therapy at the standard dose of 100 mg/day has been found to cause methemoglobinemia in 15% of patients [3]. In another case report, dapsone taken at 50 mg/day for 1 year was found to cause methemoglobinemia [3]. The purpose of presenting this case is to emphasize that dapsone can induce methemoglobinemia even at low doses taken for very short duration i.e. only for 5 days and highlight this side effect of dapsone.
Introduction
An old lady in her mid-fifties with a known case of hypothyroidism and dermatitis herpetiformis was on prednisolone for 4 years to 5 years. She has taken dapsone 2 months back only for 15 days then stopped on her own and was doing well. She again took dapsone at a dose of 50 mg per day recently for the last 5 days before the presentation. She came with complaints of cyanosis of the digits of both hands for 2 days sweating and decreased oxygen saturation for a day. She was vitally stable but her oxygen saturation w74as 85% on room air with normal arterial blood gas showing Pa02 232. She was taken on 10 liters oxygen via a non-rebreathing mask. Her cardiovascular and chest examination was unremarkable and lab workup and x-ray were normal. Since arterial blood gas was normal and all relevant workups were unremarkable, it was presumed to be dapsone-induced methemoglobinemia at a low dose and short duration. Her oxygen requirement started declining gradually and finally, she maintained oxygen saturation on room air. Dapsone-induced methemoglobinemia should be kept in mind even at low doses taken for a short period (five days) since timely diagnosis can improve clinical outcomes.
Case Presentation
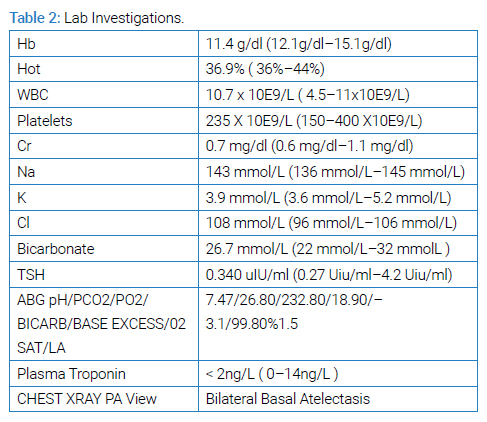
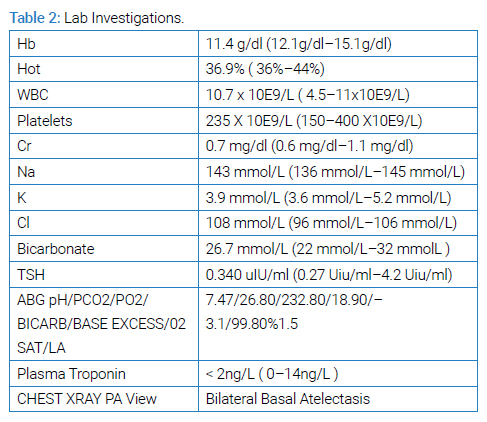
An old lady in her mid-fifties with known hypothyroid was presented to emergency with complaints of bluish discoloration of digits of both hands that developed 2 days back excessive sweating and decreased oxygen saturation for one day before presentation. She developed bluish discoloration of digits for 15 minutes to 20 minutes that resolved on its own. One day before the presentation, she developed excessive sweating while cooking in the evening for an hour. She had no associated complaint of chest pain or significant dyspnea though she had some discomfort while breathing during walking but it was relieved by resting. She got her oxygen saturation checked which was 83% on room air. She then went to a local clinic where she was taken on 5 liters to 10 liters of oxygen for one hour after which her oxygen saturation was 89% and was given injectable steroids. She came back home but at night around 3 am to 4 am her oxygen saturation again dropped to 74% on room air and she was brought to the ER. She had no other complaints of fever, cough, chest pain, sweating fatigue, etc. at the time of presentation. Her past medical history revealed that she had developed grouped excoriations, erythematous urticarial plaques, and papules with vesicles on both lower limbs and even on digits of her hand 25 years ago and had been finally diagnosed with dermatitis herpetiformis on skin lesion biopsy 6 years ago for which she has been taking tablet prednisolone 10 mg OD since 5 years. Moreover, she took a tablet of dapsone 50 mg OD for just 15 days 2 months ago for dermatitis herpetiformis and then stopped. Recently she took tablet dapsone 50 mg OD again for 5 days before presentation to ER. She also had a history of severe Covid pneumonia 2 months ago after which she took tablet prednisolone and dapsone for 15 days and then stopped. For hypothyroidism, she used to take thyroxine 50mcq QAM. On examination, she was found to have excoriated macular lesions on both her lower limbs and fingers of her hand as shown in the pictures below. She was vitally stable with no tachypnea or tachycardia but her oxygen saturation on room air was 83%. She was having bluish discoloration on the digits of both hands. The rest of the examination was unremarkable. Her celiac workup was also negative. Other lab investigations were also unremarkable as Zopiclonegiven in (Table 2). She was taken on 10-litre oxygen with a non-rebreathing mask on which she maintained saturation up to 85-86% which later gradually started improving. Her ABGs showed pH 7.47, PCO2 26.80, PO2 232.80, and bicarb 18.90 on room air. ECG as well as cardiac enzymes were normal. After a few hours, she started maintaining oxygen saturation on room air. This led to the final diagnosis of dapsone-induced methemoglobinemia even at low doses taken for a short duration.
Unfortunately, MetHb level estimation is not possible in the country. She was kept in the ward for 1 day for observation and was discharged. Her hypoxia was resolved and she was hemodynamically stable and was discharged. She was doing fine on follow-up.
Differential Diagnosis: Pneumonia was ruled out because the chest X-ray was clear and there were no infiltrates. Pulmonary embolism was clinically not suggestive. Dapsone-induced methemoglobinemia occurred after a low dose of dapsone.
Treatment: The treatment is IV methylene blue that must be given to people with symptomatic hypoxia and methylene blue levels greater than 20% at 1 mg/kg to 2 mg/kg doses every 3 minutes to 5 minutes. If it is life-threatening methemoglobinemia, then it must be treated with hyperbaric oxygen therapy.
Outcome and Follow-Up: The patient was taken on a high-low Oxygen level and she started maintaining Oxygen saturation on room air. The patient was doing quite well on follow-up (Figure).

Discussion
Dapsone has been found to cause methemoglobinemia by being metabolized in the liver via the cytochrome p450 pathway to potent oxidants that are responsible for causing methemoglobinemia [4]. The actual mechanism of dapsone-induced methemoglobinemia can be explained as in normal red blood cells cellular enzymes rapidly reduce any naturally occurring methemoglobin via e cytochrome b5-MetHb reductase pathway and pathway involving Nicotinamide Adenine Dinucleotide Phosphate (NADPH)-MetHb reductase, and exposure to oxidative medications like dapsone can overcome the role of these enzymes resulting in formation of methemoglobin [5]. The peak plasma concentration of dapsone is achieved within 2 hours to 8 hours after ingestion and varies up to 10 hours to 80 hours in cases of overdose. The typical oxygen saturation gap observed between arterial blood gas analysis and pulse oximetry is usually helpful for making a diagnosis because serum methemoglobin levels are not always immediately available, So basically the low oxygen saturation levels on pulse oximetry than arterial blood gas saturation levels indicate methemoglobinemia since it is the condition in which oxygen-carrying capacity of hemoglobin is reduced due to conversion of ferrous to ferric state [6].
According to a study by Ash-Bernal et al, the majority of the patients with methemoglobinemia were found to have dapsone as a cause of methemoglobinemia in a study involving two hospitals [4]. Regarding dosage, another retrospective analysis of 155 patients with dapsone-associated adverse effects showed 3% of patients having methemoglobinemia with dapsone given at 50 mg twice daily [4]. In another study, a greater proportion of patients treated with dapsone below the target dose of 2 mg/kg/day did not develop methemoglobinemia whereas patients given dapsone over this target dose developed methemoglobinemia [5]. The majority of studies have shown dapsone-induced methemoglobinemia after taking dapsone at high doses for a long period. Another case report and literature review showed methemoglobinemia in a lady taking dapsone for lupus at 200 mg daily 8 months before admission with the dose further increased in the last 2 months. She was then treated with methylene blue [6]. Another case study showed methemoglobinemia in a patient who had been taking dapsone for lichen planus usually at 100 mg twice a day. He landed in the hospital after taking a 1000 mg tablet at one time 6 hours before being brought in an emergency because he had not taken it for the last 3 days [7]. No study has been done so far showing dapsone-causing methemoglobinemia taken at low doses for a short period. Our case study shows dapsone causing methemoglobinemia at 50 mg once daily taken for a short period. The treatment is IV methylene blue that must be given to people with symptomatic hypoxia and methylene blue levels greater than 20% at 1 mg/kg to 2 mg/kg doses every 3 minutes to 5 minutes. If it is life-threatening methemoglobinemia, then it must be treated with hyperbaric oxygen therapy. According to a literature study, multiple doses of activated charcoal increased the elimination of dapsone. Additionally, ascorbic acid might be useful in cases where methylene blue is contraindicated like G6PD deficiency [7]. In our study methemoglobinemia levels could not be checked due to lack of facility for this test in our area. There was also another study in which definite confirmation could not be made because of the unavailability of the testing facility in Pakistan that is used to check methemoglobin levels. However, certain clues like clinical presentation, response to treatment, and arterial blood gas indicate the diagnosis. In our case, arterial blood gas was normal but pulse oximetry showed reduced oxygen saturation. The patient was managed symptomatically by administering 10 liters of oxygen via a rebreather mask. She recovered soon and started maintaining saturation on room air.
Learning Points/Take Home Messages
- Dapsone can induce methemoglobinemia in low doses taken for a short duration.
- Medication history is a critical factor to consider when making a diagnosis and ruling out other causes of methemoglobinemia.
- Methemoglobin levels are not available in Pakistan, which is a limitation for this case study; therefore, methemoglobinemia must be presumed.
Conclusion
This case report concludes that dapsone can induce methemoglobinemia at low doses taken for short period of time. The condition was mild in intensity and patient recovered with symptomatic management within 24 hours.
Keywords
Methemoglobinemia; Dapsone; Oxygen saturation gap; Dermatitis herpetiformis
Cite this article
Sana K, Sabeen A. Presumed low dose dapsone induced methemoglobinemia. World J Emerg Med Crit Care. 2024;1(1):1–4.
Copyright
© 2024 Sana Khan. This is an open access article distributed under the terms of the Creative Commons Attribution 4.0 International License (CC BY-4.0).